
5-23-2020 By Vince Giuliano with strong support from Steve Buss
This blog entry combines links to new viewpoints on the COVID-19 pandemic with interesting news, comments and strong opinions of my own.
The key points I will amplify here are:
- We – members of our species – are at war with an alien enemy species
- We are fighting that war with ancient defenses from millennia in the past
- We are losing that war which is not at all ending
- The US response to the pandemic has been particularly ineffective
- The economic damage of our approach to the Pandemic may be driving us into an economic situation as bad as or worse than the Great Depression of the 1930s
- What we have been doing about the pandemic so far has not worked well
- We have crummy tests, crummy contact tracing, and crummy control of the virus
- While the enemy virus is waging war against our species, our responses have been fragmented, different among nations, different among states in the US
- The solution to the Pandemic societal dilemma is not primarily medical
- Superb medical facilities don’t help prevent spread of the virus and the sickness and deaths which follow
- The medically-sanctioned approaches to the pandemic are not practical and are not being followed
- Tribal politics seems to dominate the public discourse Our paralysis seems to be driven by noise connected with a conflict between two major viewpoints, neither of which can work well.
- The conflict is political as well as scientific, so much as to obfuscate fact from fiction. Many special interests are involved.
- There is a better way to go
- One the key is shifting from sweeping stay shut down vs open up policies that affect everybody to focusing instead on special and intense provisions for the relatively small population of people likely to be vulnerable to the virus enemy.
- The other key is to use the tools of big-data and machine learning to find out as much as we can about ourselves to protect us against the virus.
- There are ways you can protect yourselves as an individual in the face of the pandemic
- A few relevant new research findings
- FINAL COMMENTS
- We Are At War With An Alien Enemy Species
The enemy species is of course the COVID-19 virus which is alien because it is invisible, so new and strange for us, and we are not sure where it came from. The enemy is very clever and employs stealth as a major strategy. It is hard to fight an enemy you can’t see. It is not possible reliably to tell who is infected with the virus and therefore know who to avoid to gain personal protection. The virus is highly infectious and during its incubation period infected people don’t even know they have it. A person cannot tell whether someone who seems healthy has the virus and is passing it on to him or her.
- One of these alien enemy species is real, dangerous, and strangest.


- 2. We are fighting that war with ancient defenses from past millennia
Our primary public health response has been EVERYBODY SHOULD AVOID EVERYBODY ELSE. This strategy is embodied in the strategies of social distancing, isolation and shutting down institutions and events where people interact with other people. This is a very ancient pandemic response going back to times of the Egyptian, Persian, Greek and Roman empires. One solution fits all. When in doubt, hide out. While-time honored it is a very inefficient response that does not work well with this particular COVID-19 enemy. While this approach has been widely implemented and has been used “to flatten the curve,” I think it is dumb to rely on it permanently as our main approach while we have other powerful tools available. It doesn’t work well. And it is completely toxic to our economy.
Another ancient political response to disease is denial, deliberate not-knowing. At various times, the Roman Empire used this response to deal with smallpox pandemics which devastated its armies and contributed to its ultimate demise. A good way not to register any new COVID-19 cases is simply not to test for it and pretend the Pandemic has gone away.
- We Are Losing That War Which Is Not At All Ending
Is the pandemic going away?
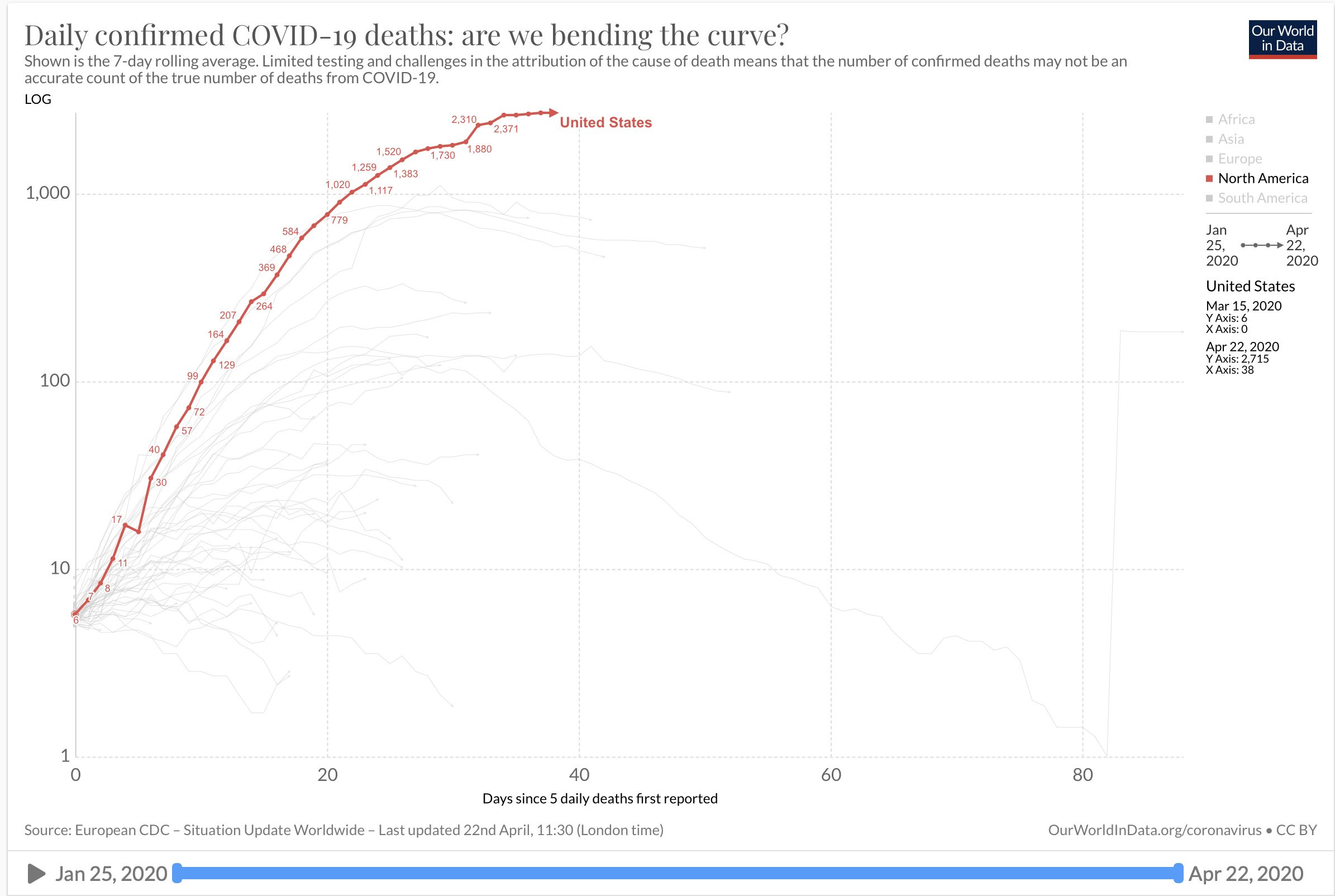
The answer is clear from this chart, which is confirmed cases and number of deaths in the US. As superman used to say, “Up. up and away.”
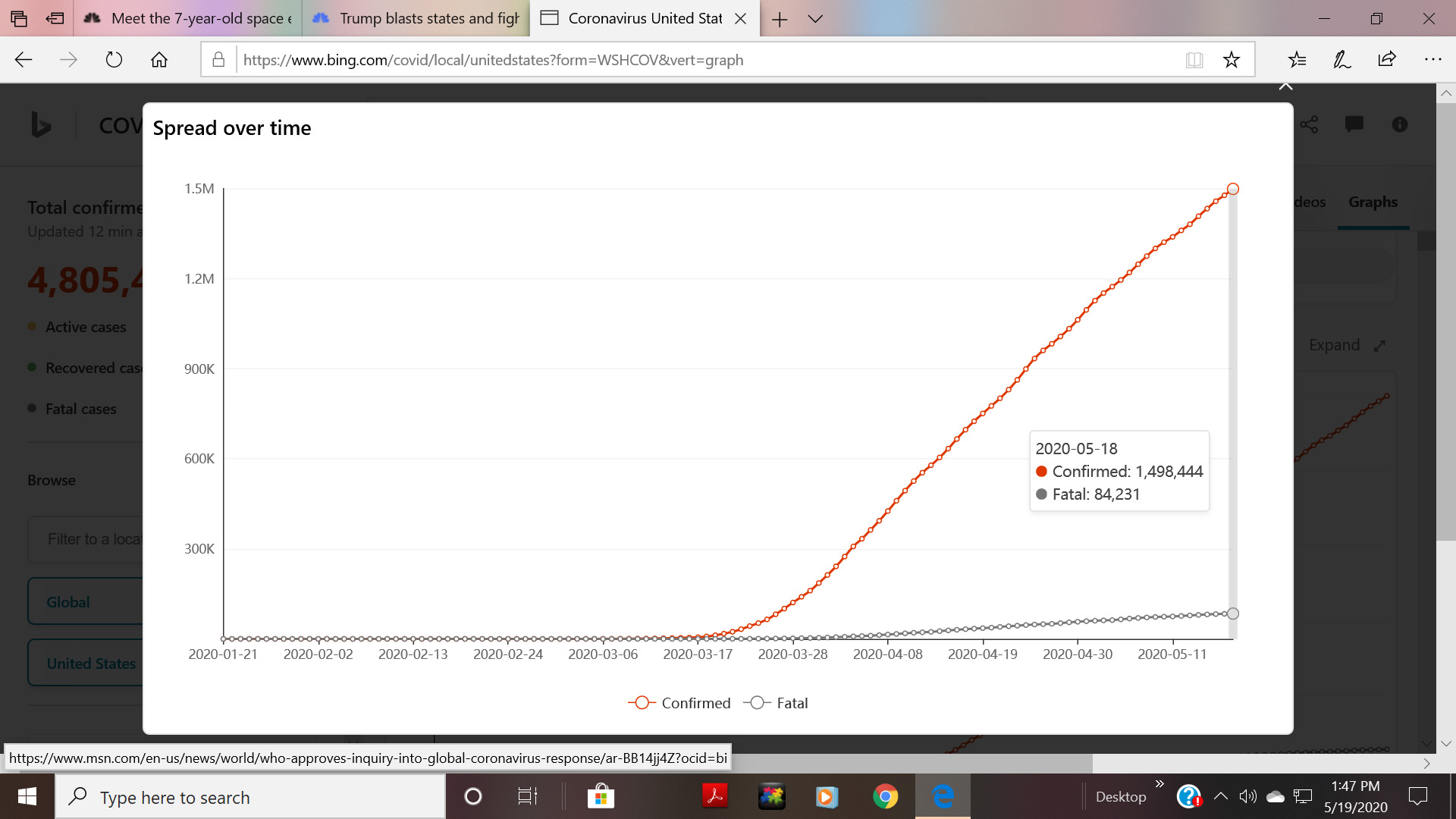
Image as of 5/19/2020
As of 5/23/2020 there were 5.2 million confirmed cases worldwide and 1.6 million in the US.(ref) Confirmed deaths from the pandemic yesterday were 383,979 worldwide and 94,722 in the US. And without doubt actual numbers of cases and deaths are much larger. By the time you read this the reported numbers will be significantly larger. At this time, the number of new cases worldwide appears to be still increasing while that in the US shows a slight tendency of leveling.
- The US response to the pandemic has been particularly ineffective
That observation is clear from looking at this chart for confirmed cases. Top green line is for the US. Lines for other countries are along the bottom See the legend shown next to the graph.
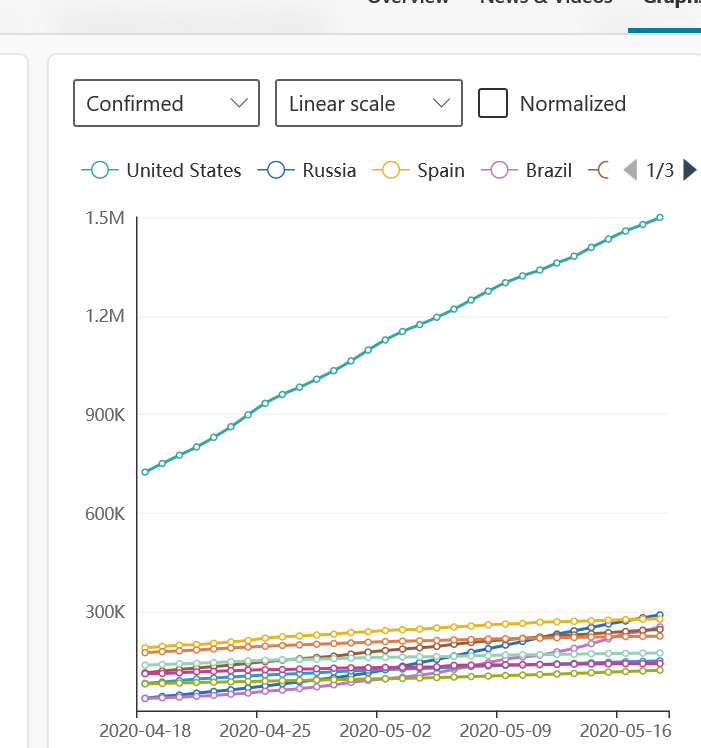
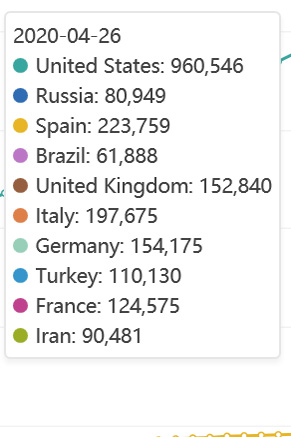
Image as of 5/19/2020
On the optimistic side we might possibly just now be peaking in death toll
But don’t be fooled by the curved look of this graph. The vertical scale is logarithmic and the actual rising death curve is still is a lot like a straight line
It is too soon to tell whether and when he virus infections will let up. Infection and death rates vary widely by country and State and from week to week. We are told additional waves of the pandemic are to be expected. A time in a war when death rates are maximal and the number of deaths is still shooting up is not a good time to declare victory. “Model Shows Increased US Deaths as Restrictions Continue to Lift. A key model used to project COVID-19 deaths in the US is now predicting more than 137,000 people in the US could die by August from the novel coronavirus. Researchers claim the augmented death toll is due to more people leaving their homes as governors relax social distancing restrictions. IHME Director Dr. Christopher Murray said in a press release that: “Unless and until we see accelerated testing, contact tracing, isolating people who test positive, and widespread use of masks in public, there is a significant likelihood of new infections.(ref)”
Renewed fears of second wave:
‘New clusters in South Korea, Germany and China show the continued risk of reopening — even in countries that are seen to have managed their outbreaks well. —  New surge in cases: There was a surge of coronavirus cases over the weekend in some of the nations around the world where stay-at-home measures and other restrictions were lifted, World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus said Monday.(ref)”
New surge in cases: There was a surge of coronavirus cases over the weekend in some of the nations around the world where stay-at-home measures and other restrictions were lifted, World Health Organization (WHO) Director-General Tedros Adhanom Ghebreyesus said Monday.(ref)”
On a very personal level, I just learned that my eldest son who is in a Massachusetts nursing home has been isolated because his routine lab tests indicate a possible COVID-19 infection.
- The economic damage of our approach may be driving us into a situation as bad as or worse than the Great Depression of the 1930s?
Economically ,we are not doing well at all in the US. We have close to 40 million unemployed people now. Perhaps many more given that informal economy numbers are not counted. See US job losses due to COVID-19 highest since Great Depression. So far the banking system as held solid, but there have been many bankruptcies with many more to come. 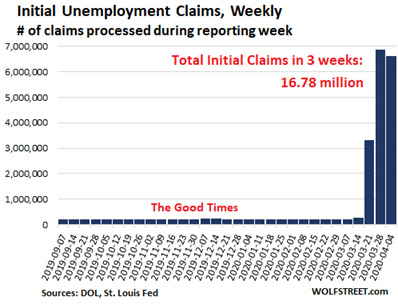 It is one thing to tell, airlines, hotels, shopping malls, cruise ships, churches, restaurants, and barbershops that they can now re-open and resume business as normal. But it remains to be seen if enough people patronize them that they can stay in business. So it may be some time before we know the extent of already-done economic damage.
It is one thing to tell, airlines, hotels, shopping malls, cruise ships, churches, restaurants, and barbershops that they can now re-open and resume business as normal. But it remains to be seen if enough people patronize them that they can stay in business. So it may be some time before we know the extent of already-done economic damage.
- What we have been doing about the pandemic so far has not worked well
This is a basic message of current data as can be seen in these and many many other current charts. Our policies have simultaneously resulted in extraordinary large number of covid-19 cases and deaths AND economic havoc.
It is generally agreed that reported case as well as death numbers are probably far below actual. The numbers of people tested for the virus who show positive in the US is probably a small fraction of those who have it or have had it. Even if someone has been tested negative, they may test positive in a few days. For the US as a whole the number of reported cases is now doubling every month, although that number varies widely by State. For Kentucky, Alabama, California, Virginia and Illinois, for example, number of cases is doubling every 3 weeks. In New York they are doubling every 3 months. (ref). But please don’t be lulled by the lower numbers; in every case they represent exponential growth, not leveling, not declining.
- We have crummy tests, crummy contact tracing, and crummy control of the virus
For months now, political leaders and media voices have been telling us that the key to controlling the virus is more and more and more tests. These tests combined with effective contact tracing for infected people should tell us who is infected and who is not. Everybody should be tested. There has been much consternation over a continuing lack of tests. But only very few people in the public sphere have been telling us about the test’s deep flaws which result in them having quite limited practical utility. Dr. Sanjay Gupta finally broke through that wall of silence this week with an article in CNN Health. There is no such thing as a standard test for COVID-19. Perhaps upwards of 100 different kinds of PCR-RT throat swab test kits are on the market, from companies in the US and around the world. Only some of these have been impartially tested and validated. Some of these produce results only after 5 days, others in a few hours, a few in 5 minutes.
The biggest problem with these tests is false negatives, where people who are in fact infected yield negative test results. False negatives can result because of improper throat swab administration, because the virus in an infected person has not yet replicated enough to show on the test, or because of flaws in the test itself. I am told by practicing clinicians that a false negative rate of 20% to 40% is not unusual. This means that 1 out of 3 or 4 tested and therefore declared to be “safe from infecting others” is in fact not safe that way at all. No wonder that a locked-down nursing home may test everybody and find one positive case who is then isolated, and test everybody again in a week and find 15 positive cases who are also quickly isolated, and the week after that test again and find 75 positive cases among patients and staff.
The serum antibody tests are completely different but also have their own problems. They are designed to look for antibodies in the blood expected to be present if a person has been infected with the virus. The antibodies are produced as part of the body’s immune system response to the virus. Mostly so, but not necessarily for everybody who has been infected. Therefore the tests are thought to possibly give us low-bound estimates of the number who have been infected. It is conjectured but not known for sure that the presence of the antibodies indicates some degree of immunity to the virus. There are also several of these tests under development and coming on the market, but some of these may also not provide reliable results. I was told by a practitioner that an imported batch of such tests showed strong positive results for people who had COVID-19 infections. But alas, the tests also showed false positive results for people who had earlier infections with other viruses like CMV, EBV and HPV. So again, you can’t conclude that a person testing positive is immune to COVID-19, because the test and presumed immunity might relate to a completely different infectious agent. And you cannot conclude that a person who has tested negative has not had the virus.
Let me be clear, I support doing a lot more testing. I think that doing widespread testing can be important for helping us guess more accurately who is vulnerable to infection with the virus and who is not. But the tests too-often don’t give correct results and mostly can’t be relied on by themselves for effective decision making.
- While the enemy virus is waging war against our species, our responses have been fragmented, different among nations, different among States in the US
While I am concentrating here on the situation in the US the Pandemic is worldwide. The virus is a war against our species although the responses to the war lacks coherency and joint international initiative. Imagine the world is under attack by a fleet of enemy spaceships and our reaction is that every nation needs defend its own citizens. And in the US, it is up to each individual State to defend itself. That is our current situation. The World Health Organization in a relatively weak voice, lacking political clout. The same can be said for the CDC in the US. Yes, medical practice seems to be international in scope and there are important philanthropies devoted to world health like the Bill and Melinda Gates Foundation. But governments seem to be the major public health actors responding to the virus in various ways and degrees.
Of course there is one major advantage to this fragmentation, and that is opportunity for learning and innovation as different approaches are being pursued and different results obtained. The value of this should not be underestimated.
- The solution to the Pandemic societal dilemma is not primarily medical
Medicine and health care is perhaps the largest sector or the US economy. However the overwhelming focus of medicine has always been the treatment of medical problems in individuals, and this usually only after symptoms of such problems have appeared. While there has been increased discussion of “preventative medicine” recently this has been secondary to what most doctors and other health care workers do. In the current Pandemic, medicine and the health care industry are only some of the key players involved -along with international meat-packing companies, nursing home operators, business owners, prison operators, cruise ship and sports team owners and politicians at every level.
Doctors and hospitals have played important roles in treating the very sick and saving a certain number of lives that would be otherwise lost. They also maintain COVID-19 patient records, conduct research studies, and disseminate medical knowledge as it is accumulated to colleagues and via research publications I believe these activities could play a very important R&D functions to help us defeat the virus. Not only potentially by creating a vaccine for COVID-19, but also by helping us understand what existing pharmaceuticals might be mobilized to blunt its deadliness. And most important of all in my mind, by helping identify biophysical properties of individuals that make them particularly more or less vulnerable in case of COVID-19 infection, More on this in Section 13 below
- Superb Medical facilities don’t help prevent spread of the virus and the sickness and deaths which follow
In health matters Massachusetts is a highly enlightened state, with hospitals, medical resources and health research programs among the very best in the world. Yet, Massachusetts had the third-highest infection and death rates from the virus in the country on a population-adjusted bases Northern Italy has one of the best medical systems in the world. Yet, the existence of that system did not prevent the wildfire spread of the virus there and the associated death rates. And statistics of death rates from the virus suggests that it sickens and kills everywhere, where there are first-class medical facilities and where such facilities don’t exist. Of course for some individuals in critical condition and threatened by death from the virus, being in a first-rate hospital might make a life-or-death difference. But from the worldwide numbers rolling in, availability of high-quality medical care does not seem to make much if any of a statistical difference. The Roman Army could not conquer smallpox, despite some Roman Emperors having ordered the Army Generals to do so. And an excellent health care system can’t conquer COVID-19, though it may contribute to saving the lives of a few of the most seriously sick.
- The medically-sanctioned approach to the pandemic are not practical and are not being followed
The central current “enlightened” proposed approach to our dilemma lacks both feasibility and imagination. For the US, that proposed solution is to double down on the conventional public health measures: My understanding is that the essence of these guidelines is:
- Vastly expand testing for the virus, to healthy but possibly exposed populations
- Get serious about 100% contacting tracing,
- Enforce strict respect social distancing,
- Keep society things closed down long and hard enough, until new cases and deaths drop down to low values
- Promulgate specific rules to be followed by specific kinds of institutions, like nursing homes, restaurants, and meat packing plants
- Fine and punish those who offend the rules,
- make sure everyone wears face masks in public, and
- accelerate work on a vaccine for the virus. And
- accept that until or unless such a vaccine is developed, the pandemic may to a significant extent be with us.
These are great ideas, and some of them seemed to have worked so far in China. But for us now in the US, they are collectively rather unrealistic – the tests are not available, sometimes require a week to get test results and often have a 30% false negative rate. Contact tracing won’t work because of possibly millions off already-infected people who we can’t identify to start with. A very large numbers of people who should know better offend the social distancing rules and won’t wear face masks. And while many companies are working hard on a vaccine for COVID-19 and here are many optimistic press releases, the best realistic scenario says this will take at least 18 months, and it may never happen. Decades of work have gone into attempting to develop a vaccine for HIV, and that has not happened yet. And the political processes and social dynamics of the moment are leading us in the opposite direction, to re-open the society. Most US States that have partially shut down are now re-opening, although they cannot assure following the guidelines for re-opening recently promulgated by the CDC. Please, we desperately need additional creativity
- Tribal politics seems to dominate the public discourse Our paralysis seems to be driven by noise connected with a conflict between two major viewpoints, neither of which can work well.
The societal shut downs in the US have of course caused economic paralysis on many fronts, leading to a political standoff that seems to me to be tribal in nature. Our paralysis seems to be driven by noise connected with a conflict between two major viewpoints, neither of which can work well. One tribe says we should keep the society mainly shut down for now to minimize deaths. And opening up social interactions too fast could lead to disastrous new virus outbreaks and much additional sickness and very many new deaths. The other tribe says not opening up our society and economy quickly and immediately could lead to massive unemployment, economic collapse and much associated suffering. I believe both sides are right in their objections. We seem to be heading to a compromise that could lead to the worst consequences of both of the two approaches.
The conflict blinds us to the fact that we, the human species, don’t have to depend only on the ancient tools of sequestering and social isolation to fight the virus. We have other very powerful tools in our tool kits, ones that most politicians and public commentators don’t realize that we have. I am talking about vast database records of the millions who have been infected by the virus and proven machine-learning software that could be applied to those database records – hopefully to enable us to predict with high certainty who among us are likely to be not vulnerable to the virus.
The conflict is political as well as scientific and commercial, so much as to obfuscate fact from fiction. many special interests are involved. An example is saliva testing kits for personal detection of infection with the virus. Early in the game the CDC was offered the option to buy such kits from several offshore suppliers. The CDC decided instead to go with a domestic supplier, knowing among other matters that a tens-of-billion dollar market was involved. The test that CDC was backing turned out not to work, so the US lost 2-3 months lead time in testing. If the pillars of our strategy is “test and isolate those who can infect others,” we had no tools to do this. And basically, we still don’t. To be clear, I don’t know what went into those early CDC decisions. But the impact may be seen in our runaway US infection rates.
- There is a better way to go – the key is shifting from sweeping stay shut down vs open up policies that affect everybody to focusing instead on special and intense provisions for the relatively small population of people likely to be vulnerable to the virus enemy
Earlier this week, Governor Charlie Baker announced a partial re-opening of businesses and institutions in my State Massachusetts. This is fine. However, I continue to think that focus on both sides of the political divide in the US is misplaced. When responsible, focus is on what to open up, when and under what conditions. I continue to think that it would be much more effective to focus on who is vulnerable to COVID-19, and seek to keep the vulnerable protected, opening up businesses and institutions of all kinds to everybody else – the vast majority of us. That is the essence of the argument Steve Buss and I put forward in the previous blog entry THE COVID-19 PANDEMIC – A THIRD WAY TO GO – CALL FOR ACTION.
That entry outlines the current social dilemma and suggests an approach for resolving it without suffering the horrible social-economic penalties of long-continuing societal and economic shutdown, or the massive hospitalizations and mega-deaths of too-rapid opening up. It involves a shift from trying to protect everyone from exposure to the virus to identifying the vulnerable given exposure, and then focus effort on protecting them. Since the vulnerable appears to be a tiny slice of the population compared to everybody, this could mean that most people could go back out and reboot our economy and society.
There, Steve Buss and I suggest a technical and societal approach which we believe might rescue us from a very profound societal dilemma we now face –A. open up our businesses and social institutions and encourage people to participate (perhaps economically and socially absolutely necessary, but could lead to millions of new cases of the pandemic and even to millions of new deaths) or B. Stay mostly closed down as we have been (could prevent a flare of new cases and may be necessary to prevent disastrous overload of our health care system, but could lead to disastrous economic collapse and tens of millions of people in our country facing starvation and great suffering.) The solution is intense analysis of existing and emerging data bases to allow us to assign Hazard Scores to individuals, which are estimates of the probability of their becoming seriously ill in case of infection with the COVID-19 virus. If this can be successfully done, people with very low Hazard Scores could be encouraged to go out back to work and into participation with others, while those with high hazard scores could be encouraged to remain sequestered at home in relative isolation.
This approach differs from the current approach in very key respects. The current approach attempts to protect everybody from getting the virus from anybody else– the approaches of quarantine and social isolation for essentially everybody. This approach necessitates shutting things down and therefore massive economic restriction. Our suggested approach is to focus protection on vulnerable individuals, those in the tiny fraction of our population who have a significant chance of getting seriously sick, require hospitalization or die if they contract the virus. Everybody else – most of us could go out to work or socialize or play, and start restoring our economy. In otherwise, focus on the problem where it is likely to be, with vulnerable people, focus less where the problem is unlikely to be, with relatively invulnerable people.
- THERE ARE ADDITIONAL WAYS YOU CAN PROTECT YOURSELVES IN THE fACE OF THE PANDEMIC
The personal risk from the pandemic in the US is generally getting worse and worse. At the same time as I write this, perhaps half of my fellow American countrymen are faced with an imminent personal decision: A. stay cloistered at home essentially quarantined from almost everybody, B, go back out in the society and perhaps to work cautiously, practicing social distancing and wearing a face mask, or C. resume what was formally for you “normal” behavior for relating to people whether working or playing. State-by-State and business-by business policy-makers are seeking to re-open society. While at the same kind new cases of COVID-19 and deaths from it in the country appear to be continuing at highest levels ever.
So, so many of us wonder: “If I go back out now and resume doing the things I used to do, what is my chance of becoming seriously ill from the disease, or of becoming one of the 1,500 of us in the US who die from it every day? I believe the decision to this key question can be based in large measure on your personal risk of getting seriously sick or confronting death if you contract the virus. Some of the information in this blog is intended to help you estimate that personal risk. The final section of this blog entry offers summaries of published medical information that can possibly help you make that decision in terms of your own personal risk factors for getting seriously sick or dying from COVID-19 should you get infected by the virus.
Key here is that the danger is not going away and death tolls are going up, not nice matters to contemplate when our emotions are screaming “Please Mommy, let me go out and play again.”
A. Personal safety generalities and for you specifically
So what else can you do to protect yourself? Multiple news sources repeat the same general wisdom about how likely you are to get sick or die from COVID-19 if you contract the virus: A. some 50% of people who test positive for it will be free of symptoms, and might not even know they are infected. B. most who get infected will not get seriously sick, though 10% to 20% might, C. As many as 1% to 2% of these people may eventually die from its complications which include acute respiratory failure, pneumonia and kidney failure. There have also been reports of longer-term consequences of virus infection, such as lung damage. These do not appear to be documented well as yet.
We have been told in many published articles that co-morbidity factors for COVID-19 include diabetes, obesity, cardiovascular and pulmonary issues, frailty, several other chronic disease conditions, and advanced age. This is a starting list of personal health red-flags suggesting limiting your public exposure. My suggestion is that if in any question, consult your physician. Other personal risk factors include the nature of your job and the degree of exposure to others your job and normal lifestyle entails. While many such risk factors have been identified, their importance has not yet been quantified. That quantification is the essence of the approach to the pandemic we are suggesting. As we see it, if your probability of getting seriously sick from Covid-19 is very small, to that extent you can consider yourself safe if you are exposed to it. I will refer to this vulnerability probability here as hazard level. Low hazard level should not be confused with immunity to the virus, which technically means something else.
B. Being Safe from Covid-19 vs. being Immune to it
We have two immune systems, a relatively fast-acting but sometimes possibly ineffective system called the innate immune system, Immunity to a virus, and a slower-acting immune system that is based on our disease experience called the adaptive immune system. The adaptive immune system maintains a database of pathogens that the body has experienced before, and is equipped with powerful tools that often can help it fight off and defeat such a re-encountered pathogen. If a virus or pathogenic microbe is recognized by that has been encountered and dealt with before, those tools are mobilized. That is what is meant by immunity. Here are resources, images and videos on the innate immune system and resources, images and videos on the adaptive immune system.
Immunity depends on pattern recognition systems and can be present to various degrees. If your body has experienced a similar pathogen, say a corona virus different than COVID-19 (there are several including ones that give you a common cold), this can possibly give you a degree of immunity to COVID-19. It is general knowledge that in a general population, about half the people who contract the COVID-19 virus are symptomless. We do not know why and don’t know if this is mainly attributable to immunity or other factors.
- Relevant new research findings
The good news in all this is that much is being learned about the COVID-19 virus and pandemic, and about us in relationship to it. Interesting new publications reporting these learnings are appearing with increasing frequency. I report on only five of these here and will probably cover others in future blog entries.
A. On hydroxychloroquine
Some small scale initial studies suggested the hydroxychloroquine may be an effective drug for lessening the impact of COVID-19 infections. Recent more-controlled and larger-scale studies say “Not at all so.” This drug is ineffective against the COVID-19 pathogen, and its widespread use may lead to twice as many deaths. Yesterday a study was published in the journal The Lancet. The results reported in this news report are “Chloroquine or hydroxychloroquine (HCQ), with or without an antibiotic, in hospitalized COVID-19 patients were associated with increased risk of death in the hospital and higher rates of arrhythmias, analysis of outcomes in nearly 100,000 patients indicated. — The 15,000 patients who received HCQ or chloroquine were about twice as likely to die compared to controls who did not receive these agents after adjusting for covariates (18.o% for hydroxychloroquine and 16% for chloroquine versus 9.3% for controls), reported Mandeep Mehra, MD, of Brigham and Women’s Hospital in Boston, and colleagues. — The drug was also associated with a higher risk of ventricular arrhythmia during hospitalization (6.1% for hydroxychloroquine, 4.3% for chloroquine versus 0.3% for controls), the authors wrote in The Lancet. Moreover, risks for both in-hospital mortality and ventricular arrhythmia were even higher compared to controls when either drug was combined with a macrolide antibiotic, they noted. — Mehra said in a statement these drugs should not be used as treatments for COVID-19 outside of clinical trials.” Again, I caution that statistical correlation is not the same as causality. For example, if hydroxychloroquine were prescribed only for those who were most desperately sick, then the enhanced death rate associated with its use would possibly reflect who it was given to, not represent causation by use of the drug. The situation is similar to that for hospital use of ventilators, where the correlation of COVID-19 patients put on hospital ventilators and mortality is extremely high (97.5% for people my age). Fact is that the ventilators themselves don’t kill the patients. It is just that they often cannot protect the people put on them because they cannot breath normally any longer.
It seems fairly clear from the data that hydroxychloroquine may be harmful and either increases or is neutral with respect to mortality associated with COVID-19. So in general, it is not a good idea to administer it except for people who need it for other reasons.
B. On Vitamin D
A May 6 2020 study suggests that insufficient level of Vitamin D may be a major risk factor associated with COVID-19 infection. The role of vitamin D in the prevention of coronavirus disease 2019 infection and mortality. “The present aim was to propose an hypothesis that there is a potential association between mean levels of vitamin D in various countries with cases and mortality caused by COVID-19. The mean levels of vitamin D for 20 European countries and morbidity and mortality caused by COVID-19 were acquired. Negative correlations between mean levels of vitamin D (average 56 mmol/L, STDEV 10.61) in each country and the number of COVID-19 cases/1M (mean 295.95, STDEV 298.7, and mortality/1M (mean 5.96, STDEV 15.13) were observed. Vitamin D levels are severely low in the aging population especially in Spain, Italy and Switzerland. This is also the most vulnerable group of the population in relation to COVID-19. It should be advisable to perform dedicated studies about vitamin D levels in COVID-19 patients with different degrees of disease severity.”
The study shows strong correlations severe vitamin D deficiency and mortality rates. The study proves little however, because it on the level of national populations where many other factors can come into play. On the other hand, the idea that Vitamin D deficiency is a co-illness and co-mortality factor for COVID-19 does not surprise me a bit. In my mind, this has been a “usual suspect” all along. At a microbiology level the theory definitely works. We know D-3 deficiency leads to chronic inflammation and numerous other disease susceptibilities. It is probably a good idea to supplement with Vitamin D-3 unless your lifestyle gives you a lot of sun exposure Especially if you are going to venture out where you may contract the COVID-19 VIRUS,
C. On taste and smell sensory loss symptoms
Sensory loss of taste and smell appears to be a screening criteria for determining whether someone with flu-like symptoms is infected with COVID-19 or some other pathogen, according to a very-recent study Association of chemosensory dysfunction and Covid‐19 in patients presenting with influenza‐like symptoms. “Background: Rapid spread of the SARS‐CoV‐2 virus and concern for viral transmission by ambulatory patients with minimal to no symptoms underline the importance of identifying early or subclinical symptoms of Covid‐19 infection. Two such candidate symptoms include reported loss of smell and taste. Understanding the timing and association of smell/taste loss in Covid‐19 may help facilitate screening and early isolation of cases. Methods: A single‐institution, cross‐sectional study evaluating patient‐reported symptoms with a focus on smell and taste was conducted using an internet‐based platform on adult subjects who underwent testing for Covid‐19. Logistic regression was employed to identify symptoms associated with Covid‐19 positivity. Results: A total of 1480 patients with influenza‐like symptoms underwent Covid‐19 testing between March 3 through 29, 2020. Our study captured 59 of 102 (58%) Covid‐19‐positive patients and 203 of 1378 (15%) Covid‐19‐negative patients. Smell and taste loss were reported in 68% (40/59) and 71% (42/59) of Covid‐19‐positive subjects, respectively, compared to 16% (33/203) and 17% (35/203) of Covid‐19‐negative patients (p<0.001). Smell and taste impairment were independently and strongly associated with Covid‐19‐positivity (anosmia: adjusted odds ratio [aOR] 10.9, 95%CI:5.08‐23.5; ageusia: aOR 10.2 95%CI:4.74‐22.1); whereas, sore throat was associated with Covid‐19‐negativity (aOR 0.23, 95%CI:0.11‐0.50). Of patients who reported Covid‐19‐associated loss of smell, 74% (28/38) reported resolution of anosmia with clinical resolution of illness. Conclusions: In ambulatory individuals with influenza‐like symptoms, chemosensory dysfunction was strongly associated with Covid‐19 infection and should be considered when screening symptoms. Most will recover chemosensory function within weeks paralleling resolution of other disease‐related symptoms.”
If you find yourself with sudden loss of taste and smell, check in with your physician
D. CAT scans appear to be the best diagnostic tool for COVID-19
I have above pointed out problems with throat-swabbing PCR tests and how very large false-negative rates make them unreliable for definitive diagnosis for infection to the virus. The best tool appears to be CT scans. Comparison of testing via PCR and via CT scans is discussed out in the publication Correlation of Chest CT and RT-PCR Testing in Coronavirus Disease 2019 (COVID-19) in China: A Report of 1014 Cases. “Background : Chest CT is used for diagnosis of 2019 novel coronavirus disease (COVID-19), as an important complement to the reverse-transcription polymerase chain reaction (RT-PCR) tests. Purpose: To investigate the diagnostic value and consistency of chest CT as compared with comparison to RT-PCR assay in COVID-19. Methods: From January 6 to February 6, 2020, 1014 patients in Wuhan, China who underwent both chest CT and RT-PCR tests were included. With RT-PCR as reference standard, the performance of chest CT in diagnosing COVID-19 was assessed. Besides, for patients with multiple RT-PCR assays, the dynamic conversion of RT-PCR results (negative to positive, positive to negative, respectively) was analyzed as compared with serial chest CT scans for those with time-interval of 4 days or more. Results: Of 1014 patients, 59% (601/1014) had positive RT-PCR results, and 88% (888/1014) had positive chest CT scans. The sensitivity of chest CT in suggesting COVID-19 was 97% (95%CI, 95-98%, 580/601 patients) based on positive RT-PCR results. In patients with negative RT-PCR results, 75% (308/413) had positive chest CT findings; of 308, 48% were considered as highly likely cases, with 33% as probable cases. By analysis of serial RT-PCR assays and CT scans, the mean interval time between the initial negative to positive RT-PCR results was 5.1 ± 1.5 days; the initial positive to subsequent negative RT-PCR result was 6.9 ± 2.3 days). 60% to 93% of cases had initial positive CT consistent with COVID-19 prior (or parallel) to the initial positive RT-PCR results. 42% (24/57) cases showed :improvement in follow-up chest CT scans before the RT-PCR results turning negative. Conclusion: Chest CT has a high sensitivity for diagnosis of COVID-19. Chest CT may be considered as a primary tool for the current COVID-19 detection in epidemic areas.”
Another study discusses ground glass opacity as a key diagnostic features seen on CAT scans: Temporal Changes of CT Findings in 90 Patients with COVID-19 Pneumonia: A Longitudinal Study. “Purpose: To perform a longitudinal study to analyze the serial CT findings over time in patients with COVID-19 pneumonia. Materials and Methods: During January 16 to February 17, 2020, 90 patients (male:female, 33:57; mean age, 45 years) with COVID-19 pneumonia were prospectively enrolled and followed up until they were discharged or died, or until the end of the study. A total of 366 CT scans were acquired and reviewed by 2 groups of radiologists for the patterns and distribution of lung abnormalities, total CT scores and number of zones involved. Those features were analyzed for temporal change. Results: CT scores and number of zones involved progressed rapidly, peaked during illness days 6-11 (median: 5 and 5), and followed by persistence of high levels. The predominant pattern of abnormalities after symptom onset was ground-glass opacity (35/78 [45%] to 49/79 [62%] in different periods). The percentage of mixed pattern peaked (30/78 [38%]) on illness days 12-17, and became the second most predominant pattern thereafter. Pure ground-glass opacity was the most prevalent sub-type of ground-glass opacity after symptom onset (20/50 [40%] to 20/28 [71%]). The percentage of ground-glass opacity with irregular linear opacity peaked on illness days 6-11 (14/50 [28%)]) and became the second most prevalent subtype thereafter. The distribution of lesions was predominantly bilateral and subpleural. 66/70 (94%) patients discharged had residual disease on final CT scans (median CT scores and zones involved: 4 and 4), with ground-glass opacity (42/70 [60%]) and pure ground-glass opacity (31/42 [74%]) the most common pattern and subtype.”
If you have good symptomatic reasons to think you might have CODID-19, particularly pulmonary ones, even if your PCR test for the virus is negative, you can ask your physician to do a chest CT scan.
- FINAL COMMENTS
The main current approaches to the Coronavirus pandemic are failing miserably. Besides the sickness and deaths and associated misery, our economic picture is probably worse than in the Great Depression of the 1930s. “Let’s stay mostly shut down and save lives’ won’t work because of unfolding economic disaster and chaos, and become the virus is likely to come roaring back when we do open up. “Let’s pretend things are back to normal and get people back working and playing again ASAP’’ won’t work when we see our health organizations overloaded, a sizable portion of our doctors and nurses, put out of commission by the virus and our loved ones sick and passing away in places where we can’t even visit them. We need something much better. We must have it.
We are in fact not helpless and I believe there is a better way
The BIG-DATA strategy we have suggested for approaching the COVID-19 pandemic is completely do-able.
- Tools of BIG DATA are here. BIG DATA ANALYSIS is at the heart of many of the fastest growing and most profitable businesses, like Amazon and Google. BIG DATA MEDICAL analysis is the probable key to Precision Medicine
- Hospital records exist for millions of people who have contracted COVID-19. These convey much information about the people in relationship to the disease, including medical records, who got seriously sick or not, who had no serious symptoms and who died. Most of these records exist in machine readable form. Stripped of patient’s names and identifiers, with proper analysis they can tell us a tremendous amount about factors making up patient vulnerability to the virus.
- Powerful computer programs for machine learning These can wade through such enormous compilations of data. There are communities of machine learning enthusiasts who regularly use them. And I bet these programs can tell us the characteristics of people who are probably vulnerable or invulnerable to covid-19, with a very high degree of statistical certainty.
The times of greatest danger are also the times of greatest opportunity
Let’s focus on how we can use the new defenses we have in our arsenal to defeat our enemy instead of having everybody trying to hide out from it. If we can succeed doing that, we can use the same defenses to recognize and defeat future pandemics as well, and the human species can emerge stronger as a result.


Pingback: Longevity Views, - Did I have a COVID-19 infection? - AGINGSCIENCES™ - Anti-Aging Firewalls™AGINGSCIENCES™ – Anti-Aging Firewalls™
I have e noted two problems with the current approach.
One is that many states and countries issue blanket orders as if the right approach in Chicago IL with it 2.7 million people, is also the right approach in Valley City IL, with a population of 13. Even the dullest of us can see the problem there. Where I live, the stay at him order was lifted before out county had a significant impact, and some chi ties in the state still had zero cases. Countries and states have an obligation to help, but the primary response has to be local to be appropriate.
The second problem is that every solution has its own mortality rate, which seems largely forgotten. One common (but somewhat dubious) statistic says there are an dutiable 40,000 deaths per year due to suicide and desperation for each 1% increase in unemployment. By that statistic, a 26% unemployment rate would correlate to a million extra deaths. While that is probably overstated, the point remains that we act as if stay at home orders and economic devastation have no human cost, but they do and it is largely ignored.
My last comment would be to point out that we have 1.36 million traffic deaths per year. Not an insignificant number compared to covid victims. Yet countries and states have never issued stay at home orders to prevent traffic accidents, Each person going on the road risks not only their life but the lives of others, so why do we treat covid as different from traffic accidents? Everyone knows the answer. Because we view the loss of freedom as more precious than the possible loss of life. We let people make their own choice about the risk to themselves and others when it comes to driving a car. Why do we then need compulsory orders for a disease? Why can’t we trust people with covid the same way we trust them in the road?