Written by James Watson, with major contributions by Vince Giuliano
Introduction – Mitochondrial Roles in the Cell
This is the second part in a series of blog entries examining the roles of mitochondria in key biological activities. For additional background information, please refer to previous writings by Vince Giuliano including the Mitochondrial Damage discussion in his aging and longevity treatise, the entry from September 12, 2012 that discusses Mitohormesis, and our December 2, 2012 blog entry on Mitochondria in health and aging, and possibilities for life prolongation – Part 1:basics. These previous entries discussed topics such as the mitochondrial damage theory of aging (i.e. the modified free radical theory of aging) the alphaproteobacteria origin of mitochondria (i.e. endosymbiotic theory), the maternal inheritance of mitochondria, mitochondrial genes in the cell nucleus (99% of genes) mitochondrial DNA (1% of genes) mitochondria anatomy, mitochondrial protein import (TIM & TOM), mitochondrial biogenesis (PGC-1α & Tfam), mitochondrial fission (FIS1 & DRP1), fusion, (MFN1, MFN2, & OPA1), oxidative phosphorylation(OXOPHOS), proton leak (mitochondrial uncoupling, thermogenesis, and hibernation, UCPs), electron leak (i.e. leaking of ROS), intrinsic control of electron leak (MnSOD and p66shc), extrinsic control of electron leak (p53/SP-1, Akt/FOXO3a and c-Myc/NF-κB) and how reducing electron leak may be a better strategy for improving health than anti-oxidant supplements (i.e. stop the leak, rather than mopping up the flood waters).
Previous blogs also discussed the “electron bottleneck” at mitochondrial Complexes I and III as the likely source for electron leak and how increasing mitochondrial biogenesis reduces electron leak by relieving this “electron bottleneck”. Most important is the concept of Mitohormesis and how low levels of escaping electrons from Complex I and III actually have a beneficial health effect via the Nrf2/Keap1 pathway. Since all of these subjects have been discussed in previous blogs, I will not re-examine these subject here except to refer to them when needed. For the reader unfamiliar with these subjects, please click on the links above for a refresher review before reading this blog.
Topics Covered in this Blog – Mitochondrial Survival and Death Pathways
In this blog, I will discuss the following key concepts of the mitochondrial responses to stress:
- Mitochondrial signaling pathways
- The role of the Mitochondrial Heat Shock Proteins
- TRAP-1 and the mitochondrial permeability transition pore (MPTP)
- The 3 Key fast acting ROS-driven responses to cellular stress
- Mitochondrial unfolded protein response (UPRmt)
- Mitochondrial specific autophagy (mitophagy)
- Programmed cell death (Apoptosis)
- Unprogrammed cell death (Necrosis)
Mitochondrial Signaling –ROS is only one of 12 signaling pathways and the “signal dose”is key to determining what “response” occurs
Mitochondrial were once thought to only function as energy factories, creating 90% of the cell’s ATP by the oxidation of pyruvate via the Krebs cycle and oxidative phosphorylation. Today we know that mitochondria perform over a dozen critical functions in health and are at the heart of over 40 human diseases. The role of mitochondria in programmed cell death (apoptosis) may be the prime function of this organelle, since it is vital to the execution of the intrinsic (mitochondria-mediated) pathway of apoptosis. The cell and the mitochondria must communicate both death signals and survival signals in a carefully orchestrated manner. For this reason, over a dozen signaling pathway shave been developed between the cell and their mitochondria. The following diagram from Pagliarini and Dixon’s review on this topic, titled Mitochondrial Modulation: reversible phosphorylation takes center stage categorizes these signaling pathways. In their article, they argue that kinases and phosphatases are the dominant method of mitochondrial signaling, but the illustration clearly shows there are many other signals as well. 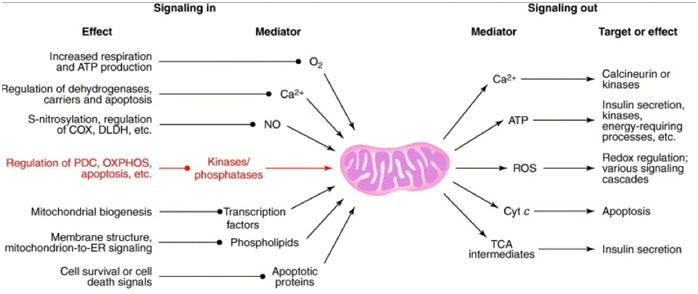
As you can see, ROS is not the only way that mitochondria communicate with the cell. Calcium is the one unique signaler that is both an “incoming signal” and an “outgoing signal” (Ca++ is how the ER communicates with mitochondria as a “cross talk” mechanism). There are other important signaling systems that are left off the diagram above, such as those initiated by misfolded proteins, damaged or mutated mitochondrial DNA, heat, hypoxia, mitochondrial toxins, ceramides, and 4-hydroxynonena. Also, the gases carbon monoxide and hydrogen sulfide are actively synthesized and function as signaling molecules at picomolar concentrations. A thorough discussion of each of these signaling molecules is beyond the scope of this blog. Instead, I will focus on the mitochondrial heat shock proteins, the mitochondrial unfolded protein response, mitochondrial autophagy (mitophagy), and the role that mitochondria play in apoptosis and necrosis. What is key to the understanding of each of these signaling pathways is the important effect of “dose” on the “response”. The same signal at low doses may have a very beneficial adaptive response, often referred to as hormesis, whereas the same signal at higher doses may trigger an unfolded protein response. At even higher doses, the same trigger may result in autophagy or even apoptosis. The following diagram nicely illustrates this “dose response” by the same cellular trigger.
| Stress Dose vs Mitochondrial Response Pathway ActivationMany mitochondrial signaling molecules can trigger different pathways at different dodes. In this theoretical diagram, hormesis refers to mitohormesis, which is the idea that at low doses, a given mitochondrial signaling molecule can mediate positive adaptive effects. (Ex: exercise, caloric restriction, etc.) At higher doses, the same signal can trigger the mitochondrial unfolded protein response (UPRmt). At even higher doses, the same molecule can trigger mitophagy. Very high doses trigger cell death via intrinsic apoptotic pathway. Pathways not shown include The MPTP & cell necrosis. |
Mitochondrial Heat Shock Response (the chaperonins)– the bidirectional “protein traffickers” between the cell and the mitochondria and their role as key stress signalers
Once thought to only function as protein folders, today the consensus is that heat shock molecules are some of the earliest signaling molecules to evolve within prokaryotic cells. The heat shock response has a much longer half life than the ROS-response pathways described in the next section, which appear to be very “fast acting”, but also much more transient in duration. Heat Shock proteins are found in the mitochondrial during non-stressed, baseline conditions, but their expressions is dramatically up regulated by three conditions: 1) physiological conditions (cell cycle division, growth factors, cell differentiation, etc.), 2) pathological conditions (viral, bacterial, and parasitic infections, fever, inflammation, ischemia, hypertrophy, oxidant injury, cancer, autoimmunity), and 3) environmental factors (heat, heavy metals, metabolic inhibitors, amino acid analogs, ethanol, antibiotics, and radiation). The heat shock proteins can be subclassified into ATP-dependent and ATP-independent HSPs. (The larger ones are ATP dependent and the smaller ones are ATP-independent). HSPs can also be classified into 3 functional groups, as follows:
1. HSPs expressed in baseline, unstressed cells – Hsp-60, Hsp-70, Hsp-90, Hsp-110
The primary role of these Hsps is protein folding, also referred to as a “molecular chaperone.”.
These HSPs are all ATP-dependet. The mitochondrial HSP60 is a member of this family.
2. HSPs expressed with glucose deprivation – Grp-34, Grp-47, Grp-56, Grp-75, Grp-78, Grp-94
These heat shock proteins also are molecular chaperones and include the mitochondrial Hsp, Grp-75 (also known as mt-Hsp70).
3. Small molecular weight HSPs – Hsp-10, Hsp-20, Ubiquitin
These heat shock proteins regulate the actin cytoskeleton (Hsp20), are involved in the nonlysosomal protein degradation (Ubiquitin), or help Hsp60 (Hsp-10)
Most of these heat shock proteins do not involve mitochondria and will not be discussed in this blog. Only 4 important heat shock proteins are commonly found in mitochondria. They are Hsp90, Hsp60, Mito-Hsp70 (Grp-75), and Hsp10. These Hsps play a vital role in mitochondria since over 1,000 proteins must be imported into the matrix, including 70 nuclear proteins needed for the respiratory electron transport chain as well as matrix proteins and factors required for mtDNA maintenance, transcription, and translation. The following diagram from Patrick Chinnnery’s review titled Searching for Mitochondrial Genes illustrates how dependent the mitochondria are on importing nuclear encoded proteins.
Mortalin (aka mitochondrial Hsp-70 or mitoHsp-70)
These imported proteins cannot pass through the two mitochondrial membranes in a folded state. For this reason, there is transporter of the outer mitochondrial membrane (TOM) and a transporter of the inner mitochondrial membrane (TIM) and two heat shock proteins are responsible for the re-folding of proteins that pass through the double mitochondrial membrane. The first Hsp to contact the imported protein is mitochondrial specific protein-folder called mitoHsp-70 or mortalin. member of the Heat Shock Protein 70 family. Mortalin/mitoHsp-70 is a heat uninducible Hsp that primarily controls cell proliferation and cellular stress. The term “mortalin”was coined because up regulation of this protein in normal cells extended lifespan and up regulation in cancer cells helped immortalized the cells. The mechanism of action appears to be associated with the perinuclear accumulation of this protein and the inactivation of p53 and Ras-Raf pathways. This seems to be a universal feature of immortalization and mortalin appears to be involved with this transformation. After a protein is imported into the mitochondrial matrix and accepted by mortalin, this Hsp passes the protein on to a mitochondrial version of Heat Shock Protein 60 (Hsp60), which completes the protein folding with the help of Hsp-10. Both Hsp-60 And Hsp-10 are heat inducible, whereas mortalin is not a heat inducible protein. This diagram from Neupert and Brunner’s article The protein import motor of mitochondria illustrates how TIM, TOM, mortalin, and Hsp-60 must work together. This process is ATP-driven through a ATP-binding to mortalin.
Mortalin – (continued)
Mortalin is also found in several extra-mitochondrial sites including the ER, cytoplasmic vesicles, and the cytoplasm. Mortalin binds to p53, membrane proteins such as FGF1, IL-1α, cytoskeleton proteins, and p66shc (a controller of ROS levels in mitochondria). In this extra-mitochondrial role, mortalin is a “pro-survival chaperone” that is anti-apoptotic. It is one of the most important antiapoptotic genes in that it protects the cell from many different stressors, including arsnite, glucose starvation, ischemia-reperfusion, etc. With UV-light exposure, mortalin releases the transcription factor p66shc , which triggers collapse of the mitochondrial membrane potential (ΨP), increasing “ROS” production. Two apoptosis pathways are inhibited by mortalin: 1) Fas receptor engagement with its ligand, the N-terminal portion of the cyclin-depedent kinase 11 (CDK11-p60), results in its translocation from the nucleus to the mitochondria where it associates with mortalin, thereby preventing apoptosis. 2) p53 also translocates from the nucleus to the mitochondria to trigger apoptosis, but mortalin binds the translocated p53, preventing apoptosis.
Mitichondrial Hsp-60
Although Hsp60 was once thought to be mitochondrial specific, but non-mitochondrial homologs of Hsp-60 have been found outside mitochondria and it is no longer considered to be mitochondrial specific. Hsp-60 can be found in other locations in the cell and this appears to be a signaling role for Hsp-60. Hsp-60 may also play a role in the development of insulin-dependent diabetes by its role in insulin secretory granuales. Hsp-60 also forms a complex with histone 2B. Both mortalin and Hsp-60 are found on the surface of cancer cells (but not on normal cell surfaces).
Signaling proteins are exported from the mitochondria. For this to happen, they must be unfolded, passed through the double membrane, and then be re-folded in the cytoplasm by a cytoplasmic version of Hsp-60. With the Hsp-60 family having many unique members now identified, it is believed that the Hsp-60 family folds between 15-30% of the total proteins found in the cell. Hsp-60 has a co-chaperone called Hsp-10. Both of these are heat inducible. Hsp-60 and Hsp-10 are both pro-apoptotic and anti-apoptotic. Over-expression of the Hsp-60/Hsp-10 complex protects cells from ischemia and from chemotherapy induced apoptosis when mitochondrial membranes are intact. However when the outer mitochondrial membrane is disrupted in apoptosis, the released Hsp-60/Hsp-10 complex activates caspace-3, thereby becoming a pro-apoptotic factor.
Longevity, Cellular Senescence, Chemotherapy resistance of cancer, and Heat Shock Proteins
Heat shock proteins play an important role in aging and cellular senescence. Although Hsp-60 does not extend lifespan, mortalin overexpression extends lifespan in human fibroblasts, increasing population doublings before senescence occurs. This apparent “dominance” of mortalin may be due to the fact that mortalin must first accept the imported proteins before Hsp-60 can handle them. Chemotherapy resistance also appears to be due in part to the anti-apoptotic roles of Hsp-90, Hsp-27, and Hsp-70. Mortalin plays a role here as well, as a mitochondrial-specific Hsp-70, but the exact mechanism of action is not known.
Hsp-90 and Mitochondria
HSP-90 is also found in the mitochondria but is not unique to the mitochondria. Hsp-90 is present in the mitochondrial under unstressed conditions, but is dramatically up regulated with cellular stress. In cancer cells, mitochondrial Hsp-90 is dramatically up regulated (along with TRAP-1). In the cytoplasm, Hsp-90 plays an important role in binding to steroid receptors, preventing steroid hormones from binding. In this aspect, Hsp-90 reduces the function of corticosteroids on gene expression. In recent years, another heat shock protein that plays a central role in mitochondria has been discovered. This new chaperone is similar to Hsp-90 and is called the TNF receptor- associated protein-1, or TRAP-1. The following section will describe it’s crucial role in stabilizing the integrity of the inner mitochondrial membrane by blocking the opening of the mitochondrial permeability transition pore (MPTP).
Proteins are exported out of the cytoplasm for signaling purposes as well. It appears that a cytoplasmic version of Hsp-60 is needed for re-folding of the exported protein. With the Hsp-60 family having many unique members now identified, it is believed that this protein folding family folds between 15-30% of the total proteins found in the cell. Hsp-60 has a helper, called Hsp-10. HSP-90 is also found in the mitochondrial but is not unique to the mitochondria. Hsp-90 is present in the mitochondrial under unstressed conditions, but is dramatically up regulated with cellular stress. In cancer cells, mitochondrial Hsp-90 is dramatically up regulated (along with TRAP-1). In the cytoplasm, Hsp-90 plays an important role in binding to steroid receptors, preventing steroid hormones from further binding. In this aspect, Hsp-90 reduces the functionung of corticosteroids on gene expression. In recent years, another heat shock protein that plays a central role in mitochondria has been discovered.
TRAP-1 and the Mitochondrial Permeability Pore (MPTP) – TRAP-1 is the “master mitochondrial chaperone” and the MPTP is the “necrotic death pathway” mediator
Unlike most of the mitochondrial-specific heat shock proteins described above, there is a Hsp-90 homolog, called TNF receptor–associated protein-1 (TRAP-1). Although TRAP-1 has been found in other locations in the cell, it’s “home base” is now thought to be the mitochondrial matrix. Whereas TRAP-1 levels in unstressed cells are low, TRAP-1 levels dramatically increase with cellular stress. For instance, in cancer cells TRAP-1 levels are up regulated and inhibit cancer cell apoptosis, suppress ROS production by the mitochondria, and are responsible for cancer. chemotherapy resistance. This effect is probably mediated by TRAP-1 stabilization of the inner mitochondrial membrane by preventing the opening of the mitochondrial permeability transition port (MPTP), which is a large channel pore found only in the inner mitochondrial membrane made up by a protein called Cyclophillin D. High calcium levels trigger opening of the MPTP, which results in disruption of the inner mitochondrial membrane and a rapid influx of water and solutes, causing the matrix volume to increase. TRAP-1 forms a complex with Hsp-60, Hsp-90 and the pore protein Cyclophillin D, effectively preventing the pore from opening. The following diagram from Lucia Languino (et.al.) 2012 article TRAP-1, the mitochondrial Hsp 90 illustrates the way that Hsp90, Hsp60, and TRAP-1, block the Cyclophillin D protein of the MPTP.
This results in protection from the inner mitochondrial death pathway called the mitochondrial permeability transition (MPT), which is the phenomena for which the MPTP is named after. Thus, TRAP-1 (with its cohorts, Hsp-60 and Hsp-90) confers cytoprotection to stress and increases cell resistance to necrosis and apoptosis. TRAP-1 cytoprotection is further augmented by PINK1 phosphorylation of TRAP-1, which increases apoptosis resistance, reduces ROS production, and increases drug resistance to chemotherapy even more. The following diagram illustrates the effects of PINK1 on the mitochondrial pathways:
High ROS or cardiolipin, low levels of spermidine or low mitochondrial membrane potential (ΔΨ) all exacerbate calcium-induced MPTP opening. If only the inner mitochondrial membrane is disrupted, only the mitochondria dies (mitoptosis). If the swelling is too severe, the outer mitochondrial membrane ruptures, spilling out cytochrome c triggering apoptosis. If both the inner and outer mitochondrial membrane are ruptured in short order, a rapid cell death by necrosis occurs. This appears to be the mechanism by which cardiomyocytes die in a heart attack or how neurons die in an occlusive stroke. Blocking the heat shock proteins that prevent the MPTP channel from opening is a potential strategy for killing cancer cells. Gamitrinib, a Hsp90/TRAP-1 inhibitor, makes cancer cells more sensitive to apoptosis, triggers autophagy, and increases gene expression for the mitochondrial unfolded protein response (UPRmt). The following diagram from Languino (et.al.) 2012 article TRAP-1, the mitochondrial Hsp 90 illustrates the 3 responses to TRAP-1 inhibition by Gamitrinib.
Conclusions on TRAP-1: The mitochondrial heat shock protein TRAP-1 is a mitochondrial matrix protein that appears to be the master controller of fate in mitochondria, much like p53 is the master controller in the cell nucleus. Under normal conditions, TRAP-1 is down regulated and found in low concentrations at the inner mitochondrial membrane, where TRAP-1 controls the opening of the mitochondrial permeability transition pore (MPTP). Phosphorylation of TRAP-1 by PINK1 increases the activity of TRAP-1 making the cell more resistant to stressors. High levels of calcium activate the opening of the MPTP, allowing solutes and fluid to rush through the inner mitochondrial membrane and into the mitochondrial matrix, causing the matrix space to swell. If the damage is limited to the mitochondria and the outer membrane does not rupture, only mitoptosis occurs. If the damage is too severe, the outer mitochondrial membrane ruptures, triggering apoptosis. In this case, the cell dies. In cancer, TRAP-1 is upregulated, making cancer cells resistant to chemotherapy and apoptosis. Upregulating TRAP-1 also reduces ROS levels by unknown mechanisms, but is likely to be due to reducing electron leak from the mitochondria. These effects of increased TRAP-1 are responsible for cancer cell survival.
Increasing TRAP-1 can also be accomplished with stress pre-conditioning using the same principles applicable to mitohormesis. (exercise, heat, cold, CR, fasting, and hypoxic stress preconditioning). By preconditioning cells to stress, it is possible to reduce the necrosis and reperfusion injury in head trauma, stroke, myocardial infarction, and other severe acute conditions, increasing the chance of surviving these events. This TRAP-1 mechanism is therefore an important stress response that we should exploit to promote health and resist disease
The Three Key Fast Acting, ROS-driven Responses to Cellular Stress
In the past 20 years, there is a large body of experimental evidence for the 3 “fast acting stress response” pathways that can be activated much faster than the Heat Shock Response. With these 3 pathways, there are “pre-synthesized transcription factors” located in the cytosol that quickly migrate to the nucleus to turn on hundreds of stress-response genes. (With the heat shock response, the transcription factors have to be synthesized). These three pathways are triggered by infection, UV light, hypoxia, toxic metals, ROS, and RNS and are mediated by three transcription factors and the inhibitor that holds them in the cytosol: Nrf2/Keap1, NF-kB/IKBα, and HIF-1α/VHL. The diagram below from Qiang Ma’s 2010 article titled Transcriptional responses to oxidative stress nicely illustrate these three fast acting responses to stress:
The 3 ROS-mediated Responses to Cellular StressStressors can turn on a wide variety of genes using ROS as second messengers to activate transcription factors located in the cytoplasm. Although many stressors can activate these pathways, the common trigger or mediator is ROS, generated by the plasma membrane redox system or mitochondrial OXPHOS system. The pathways are NF-kB, Nrf2, & HIF-1a.NF-kB pathway: Phosphorylation of inhibitor protein, IkBα leads to the ubiquitination and proteasomal degradation of IκBα through the Cul1-dependent SCF E3 complex. This frees NF-κB to migrate into the nucleus, turning on genes that cause inflammation.Nrf2 pathway: Free radicals and other electrophiles bind to critical cysteine thiol groups of inhibitor protein Keap1 (and Nrf2) resulting in the inhibition of ubiquitination–proteasomal degradation of Nrf2. This allows Nrf2 to mitgrate into the nucleus and turn on genes for the antioxidant response elements (ARE), which up regulated ROS scavengers and detoxifying enzymes.HIF-1α pathway:When oxygen levels are normal, two proline residues of HIF1α are converted to hydroxyproline that is recognized by VHL. VHL targets HIF1α for ubiquitination–proteasomal degradation. Hypoxia reduces this process and allows HIF1α to migrate into the nucleus, turning on genes to cope with hypoxia.Mitochondrial Unfolded Protein Response – the UPRmt Higher levels of mitochondrial stress trigger a different pathway that shares some similarities to the cytoplasmic heat shock protein pathway (HSP) and the ER unfolded protein response UPRER. The mitochondrial heat shock pathway is called the mitochondrial unfolded protein response or UPRmt. The UPRmt is really a signaling pathway that allows the mitochondrial “to tell the cell nucleus” to turn on genes required for relieving mitochondrial protein stress – mitochondrial chaperone proteins and mitochondrial proteases. Since there are two spaces in the mitochondria that can be stressed, (matrix and intermembrane space), there are two mitochondrial-to-nuclear signaling pathways: The JNK2 pathway (for signaling protein stress from the mitochondrial matrix) and the AKT pathway (for signaling protein stress from the IMS). The JNK2 kinase triggers the transcription factor, CHOP (by a complex pathway involving c-Jun and AP-1), which then translocates into the nucleus to trigger genes for quality control proteases (ClpP) and for chaperone proteins (Hsp60). The AKT kinase triggers phosphorylation of the estrogen receptor, ER?, inducing gene transcription for the IMS proteinase (Htra2) and for the transcription factor Nrf1. The following diagram illustrates this mitochondrial-to-nuclear signaling from Haynes article titled Signaling the mitochondrial unfolded protein response. 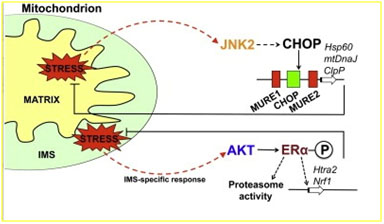
The UPRmt is normally triggered in health by heat (protein unfolding), but this response is transient since The UPRmt works to correct the protein misfolding problem. Toxic chemicals can also trigger the UPRmt such as ethidium bromide (which is used in experiments to kill all of the cells mitochondria by inhibiting mtDNA replication) and insecticides (Ex:paraquat) which also can destroy mitochondria by producing excessive ROS. Mutant mitochondria which produce excessive levels of ROS also trigger the UPRmt. These includes mitochondria in inherited mitochondrial mutation diseases as well as mutant mitochondria in aging cells. Since ROS/RNS levels are much higher in such incidences than hormetic doses, mitochondrial-specific anti-oxidants such as (EPI-743) may play a role in arresting some of the disease progression and may even reverse symptoms in patients with mitochondrial mutations such as in Leber’s hereditary optic neuropathy and Leigh Syndrome. Here are some other mitochondrial-specific substances which may help treat diseases where the UPRmt is activated: melatonin, Coenzyme Q, NAC, L-carnosine, SkQ1, and C60 fullerenes in olive oil. Spastic paraplegia – This is a neurodegenerative disease than can be caused by 13 different mutations involving mitochondrial chaperone proteins or mitochondrial protease genes. First the UPRmt is triggered, but the response does not correct the protein stress. Eventually the mitochondria trigger neuronal apoptosis. There is some evidence that mitochondrial-specific antioxidants may help alleviate or delay the progression of symptoms in this incurable, untreatable condition. Fredreich’s ataxia (FA) – This is another neurodegenerative disease, due to a trinucleotide expansion in the gene coding for the protein frataxin. This is an iron-sulfur complex cluster protein found in mitochondria that is critical for mitochondrial biogenesis and intracellular iron homeostasis. Several cytoplasmic and nuclear proteins involved with DNA repair also need these iron clusters. As a result both the cytosolic and UPRmt are activated in Fredreich’s ataxia. An interesting note is that EPI-743, a synthetic mitochondrial-specific anti-oxidant, dramatically reduced or delayed the symptoms of the disease when administered early in life. Cancer – Many cancers have an activated, upregulated UPRmt response. In most all cases, this is due to point mutations in mitochondrial genes or nuclear genes, as well as aneuploidy. Some of these mutations appear to cause cancer and others merely enhance tumor growth. In most cancers, reduced aerobic respiration occurs, leading to increased glycolysis. This is called the Warburg effect and may be due in part to damaged mitochondrial triggering the UPRmt. In most all cases, there is increased ROS and genomic instability. It is still unclear which is the “cause” and which is the “effect” in cancer cells. Most believe that mitochondrial-specific antioxidants may help cancer cells survive in these situations. Aging – Aging is associated with the accumulation of misfolded proteins in the mitochondria and proteins damaged by ROS and RNS. Although there may be disease-specific deficits, aging and age-related diseases have functionally impaired mitochondrial-specific proteases, especially the Lon protease system, found in the mitochondrial matrix. Once the Lon protease system in mitochondria is no longer functional, the UPRmt is chronically activated in aging. This is a pathologic condition, since the UPRmt is not normally continuously activated. Unfortunately, this is not a problem that can necessarily be “fixed” by nuclear gene expression. Conclusions regarding UPRmt: When mitochondrial stress levels supercede hormetic doses, the UPRmt may be the next pathway triggered by increasing doses of ROS, RNS, hypoxia, heat, and toxins. This response attempts to repair the loss of protein homeostasis in the mitochondria by up regulating both chaperone proteins and proteasomes found in the mitochondria. Most diseases where mitochondrial DNA is mutated have up-regulated UPRmt. In aging, the Lon protease system in mitochondria is functionally impaired, resulting in chronic UPRmt activation. The dysfunctional Lon protease problem cannot be repaired simply with JNK2 and AKT signaling with nuclear gene upregulation. If the mitochondrial damage cannot be repaired, the next pathway to be triggered is mitophagy. I discuss this pathway in the following section. Mitophagy – The 1st mitochondrial response to “unrepairable damage” When mitochondrial stress levels increase and the UPRmt cannot repair the damage, a specific form of autophagy occurs called form of autophagy occurs called mitophagy. Non-selective autophagy occurs when cells are deprived of nutrients and this process degrades many organelles and proteins found in the cytoplasm, including the golgi apparatus, endoplasmic reticulum, vesicles, cytoskeleton components ((microtubules and microfilaments), and any protein complexes. With non-selective autophagy, an autophagosome forms with these structures inside and this fuses with a lysosome for degradation inside the cell. This is essentially the “recycling system” of the cell and the amino acids, fatty acids, and other molecular building blocks salvaged can be used for providing energy (ATP production) or to create new macromolecular structures. Mitophagy, on the other hand, is mitochondrial-specific and is thought to occur only for regulating mitochondrial number or to selectively remove damaged mitochondria. When mitochondria are damaged, a kinase PTEN-induced putative kinase protein 1 (PINK1) accumulates and recruits Parkin, a cytosolic E3 ubiquitin ligase with 2 RING fingers, which “tags” the damaged mitochondria with ubiquitin. The ubiquitin triggers a membrane to form around the mitochondria similar to the formation of an autophagosome in non-selective autophagy. This membrane enclosed mitochondria then fuses with a lysosome where it is degraded. The two diagrams below illustrate the difference between mitophagy and non-selective autophagy, and also show the role of PINK1, Parkin, and ubiquitin in mitophagy. This is essentially the “recycling system” of the cell and the amino acids, fatty acids, and other molecular building blocks salvaged can be used for providing energy (ATP production) or to create new macromolecular structures. Mitophagy, on the other hand, is mitochondrial-specific and is thought to occur only for regulating mitochondrial number or to selectively remove damaged mitochondria. When mitochondria are damaged, a kinase PTEN-induced putative kinase protein 1 (PINK1) accumulates and recruits Parkin, a cytosolic E3 ubiquitin ligase with 2 RING fingers, which “tags” the damaged mitochondria with ubiquitin. The ubiquitin triggers a membrane to form around the mitochondria similar to the formation of an autophagosome in non-selective autophagy. This membrane enclosed mitochondria then fuses with a lysosome where it is degraded. The two diagrams below illustrate the difference between mitophagy and non-selective autophagy, and also show the role of PINK1, Parkin, and ubiquitin in mitophagy. Reference for both illustrations: Youle and Narendra, Mechanisms of Mitophagy, Nature Reviews, January, 2011. Mitophagy is a very effective mechanism for “clearing out bad mitochondria” if it is working right. The following illustration shows how mitochondrial fission and fusion can work together to “weed out” bad mitochondria. This is why mitophagy is so important in maintaining cell health. When PINK1 or Parkin are mutated, as they often are in hereditary Parkinson’s disease, the consequences are devastating. The following illustration is from Imai and Lu’s review of Parkinson’s disease.
The “ROS Paradox of Mitophagy Control — High ROS and RNS pardoxically inhibit mitophagy by interacting with cysteine residues on Parkin Mitophagy is triggered by unrepairable mitochondrial damage and is mediated by PINK1 and Parkin. Caloric restriction also triggers mitophagy and this is one of many mechanism by which (caloric restriction) extends lifespan in lower life forms. Several specific pathways within the cell inhibit mitophagy (Insulin/IGF-1 pathway and mTOR pathways are the two most important). Mitophagy is nature’s way of “clearing out bad mitochondria”. Since bad mitochondria produce higher than normal levels of ROS, mitophagy is an excellent way of getting rid of high ROS and RNS levels. Unfortunately, high levels of ROS and RNS can backfire and inhibit mitophagy, rather than activating mitophagy. This occurs because the E3 Ligase, Parkin, has several cysteine side chains (thiol groups) on the enzyme which are very sensitive to ROS and RNS. When these cysteine side chains interact with free radicals, this inactivates Parkin and Parkin aggregates, due to low solubility. This may be one of the reasons why high levels of ROS or RNS prevent mitophagy, rather than activate mitophagy. What happens instead of mitophagy is cell death, cancer, or cellular senescence. The following illustration is from Kirkin and Dikic’s review titled Ubiquitin Networks In Cancer.
Mitophagy, Mitochondrial Fusion, Mitochondrial Fission, and mitochondrial motility (microtubule transport) must be discussed together when it comes to the discussion of disease, since they all are interrelated. The following hypothetical diagram illustrates how specific defects in these four mitochondrial dynamics can lead to disease (from Chen and Chan’s 2009 article titled Mitochondrial dynamics – fusion, fission, movement, and mitophagy – in neurodegenerative Diseases.)
From the same publication: “Neurons are metabolically active cells with high energy demands at locations distant from the cell body. As a result, these cells are particularly dependent on mitochondrial function, as reflected by the observation that diseases of mitochondrial dysfunction often have a neurodegenerative component. Recent discoveries have highlighted that neurons are reliant particularly on the dynamic properties of mitochondria. Mitochondria are dynamic organelles by several criteria. They engage in repeated cycles of fusion and fission, which serve to intermix the lipids and contents of a population of mitochondria. In addition, mitochondria are actively recruited to subcellular sites, such as the axonal and dendritic processes of neurons. Finally, the quality of a mitochondrial population is maintained through mitophagy, a form of autophagy in which defective mitochondria are selectively degraded. We review the general features of mitochondrial dynamics, incorporating recent findings on mitochondrial fusion, fission, transport and mitophagy. Defects in these key features are associated with neurodegenerative disease. Charcot-Marie-Tooth type 2A, a peripheral neuropathy, and dominant optic atrophy, an inherited optic neuropathy, result from a primary deficiency of mitochondrial fusion. Moreover, several major neurodegenerative diseases—including Parkinson’s, Alzheimer’s and Huntington’s disease—involve disruption of mitochondrial dynamics. Remarkably, in several disease models, the manipulation of mitochondrial fusion or fission can partially rescue disease phenotypes. We review how mitochondrial dynamics is altered in these neurodegenerative diseases and discuss the reciprocal interactions between mitochondrial fusion, fission, transport and mitophagy.” The following diagram from Chen and Chan’s 2009 article shows where the anatomical loss of neurons occurs in six different neurodegenerative diseases where mitochondrial dynamics are altered. Charcot Marie Tooth Type 2A disease and Dominant Optic Atrophy are primarily defects in mitochondrial fusion. Hereditary forms of Parkinson’s disease either have defects in mitophagy (Parkin mutations) or are still poorly understood (PINK1 mutations). Although abnormal mitochondria are seen in Alzheimer’s disease, it is unclear what is the specific mitochondrial dynamic problem. Amyloid-? localizes to mitochondria and appears to be toxic to mitochondria. Animal models of AD have increased mitochondrial fission, although it is unclear if this occurs in human clinical disease. Huntington’s disease appears to be a disruption of fission and fusion by the mutant form of Huntington protein. There are several practical approaches to positively changing mitochondrial dynamics (including fission, fusion, Mitophagy, etc.) Although I do not like lists (since lists do not illustrate overlaps, like Venn diagrams), I will use the list format for the sake of clarity and simplicity. Coupling Mitophagy and Mitochondrial Biogenesis – making sure mitochondrial depletion does not occur Mitophagy and mitochondrial biogenesis are closely coupled to avoid mitochondrial depletion and cell death. Excessive autophagy without mitochondrial biogenesis overstresses the remaining mitochondria, triggering apotosis. This may be why fasting (or caloric restriction) up regulates both mitophagy and mitochondrial biogenesis. Mitochondrial biogenesis is primarily controlled by a co-activator, not a transcription factor. This transcriptional co-activator is called peroxisome proliferator-activated receptor-? co-activator 1? (PGC-1?). See this blog entry, this one, and this one. Mitophagy is primarily controlled by Parkin, an E3 ubiquitin ligase. Parkin activity can indirectly control PGC-1? via zinc finger protein PARIS (ZNF746), which binds to the insulin response sequence of the PGC-1? promoter. This is how mitophagy and mitochondrial biogenesis are coupled to avoid mitochondrial depletion and cell death. Altering Mitochondrial Dynamics – practical and theoretical strategies to get rid of bad Mitochondria and promote good mitochondria by upregulating mitophagy, inhibiting fission, gene repair, and mitochondrial transplantation (cytoplasmic transfer) There are several practical approaches to positively changing mitochondrial dynamics (including fission, fusion, Mitophagy, etc.) Although I do not like lists (since lists do not illustrate overlaps, like Venn diagrams), I will use the list format for the sake of clarity and simplicity. 1. Caloric Restriction and Fasting – These strategies increase mitophagy (via down regulating Insulin-IGF pathway, inhibiting mTOR), SIRT1-mediated deacetylation (and activation) of multiple transcription factors. Caloric restriction or fasting also increases mitochondrial biogenesis via PGC-1?. This strategy works well in healthy, young cells without inherited mtDNA mutations, but does not work as well with 2. Upregulating PGC-1? – this is a strategy to increase mitochondrial biogenesis. This can be done by caloric restriction, exercise, SIRT activators, phytochemicals, and several pharmaceutical drugs. Although this may appear superficially to be a futile, method since it would in theory upregulate both mutant (damaged) and wild type mitochondria, studies have shown that it appears to decrease the stress on the remaining healthy mitochondria and protect against age-related mitochondrial dysfunction in muscles..Several PGC-1? agonists have been developed, including benzafibrate, irisin, pyrroloquinoline quinone (PQQ), and GW-501516. See the blog entry PQQ – activator of PGC-1alpha, SIRT3 and mitochondrial biogenesis. 3. Upregulating AMPK – The beneficial; effects of exercise are primarily mediated via AMPK. This has been discussed in the blog AMPK and longevity. AMPK can also be up-regulatedby acadesine, metformin, GW-501516, AICAR 4. mTOR inhibition – One of the most significant measurable effects of mTOR inhibition is the up-regulation of mitophagy. Rapamycin, the bacterial secretory product from soil bacteria found on Easter Island has gained a lot of attention over the past 10 years for its effects on preventing age-related problems such as cellular senesecence as well as preventing cancer. These effects are thought to be mediated via inhibition of the mTOR pathway, which inhibits mitophagy. Inhibiting the mTOR pathway has been discussed in several previous blog entries including The many faces of mTOR and rapamycin, Longevity genes, mTOR and lifespan, Viva mTOR! Caveat mTOR! and More mTOR links to aging theories. Because of its anti-cancer and other health and longevity-producing properties, rapamycin analogs (rapalogs) have been developed by pharmaceutical companies. 5. Mitochondrial-specific antioxidants – There are several mitochondrial-specific antioxidants that may help control the suprahormetic doses of ROS seen with mitochondrial dynamics dysregulation in large doses, based on in vivo animal models. Vitamin C, the B complex viatmins, and vitamin K are also antioxidants but are not mitochondria-specific and have not been shown to be that effective. 6. Inhibiting mitochondrial fission – Mitochondrial fragmentation is usually a function of OXPHOS dysfunction (i.e. electron transport is dysregulated and there is a lot of “electron leak”). As a result the balance of fission and fusion is often tipped towards fission. Recently a “fission inhibitor” has been discovered called mdivi-1 (mitochondrial division inhibitor 1). This prevents the function of DRP1 which acts as the “noose” to divide mitochondria. This holds a lot of promise for Charcot Marie Tooth type 2A and OPA1. It may also work for some other neurodegenerative diseases such as AD or PD, and also for aging. It will not work for the 200+ mitochondrial mutation diseases, however. 7. Modulating aberrant Calcium homeostasis – A common feature of mitochondrial disease is abnormal calcium homeostatis. Recently mitochondrial-specific calcium channel blockers have been shown to be effective in correcting this problem. (CGP37157). Another calcium channel blocker called isradipine, an old hypertension drug, has shown promise for treating Parkinson’s disease-associated mitochondrial dynamics. This is more of a “treating the symptom” approach, other than treating the underlying disease, but it so simple that it holds a lot of promise for aging and for neurodegenerative diseases. Again, it is unlikely to help with mitochondrial mutation diseases. 8. Glucose depletion and ketogenic diet – Mitochondrial heteroplasmy refers to the cellular phenotype where there exists a population of normal mitochondria (wild type) and mutated mitochondria (mtDNA mutations). This scenario occurs in several inherited disorders, but also occurs with aging. In in vitro studies of artificially created cybrid cells (cells with mitochondrial heteroplasmy), a glucose-depleted, ketongenic cell media promoted an increase in wild type mitochondria and decreased the proportion of mutant mitochondria. A ketogenic diet is one that features keytone bodies as energy sources rather than glucose and involves metabolism in the cytoplasm instead of in mitochondria. Glucose inhibitors such as 2-deoxyglucose which prevent glycolysis and are “calorie restriction mimetics” have also been shown to select for health mitochondria and to get rid of damaged mitochondria. This effectively was a “dietary induction of selective mutant mitophagy,” which is what one would expect based on what has been discussed previously in this blog. 9. Gene therapy with a mitochondrially-targeted Zinc finger nuclease – Zinc finger nucleases are very specific DNA binding synthetic nucleases that can be made based on zinc finger endonuclease design. Their specificity is due to their histidine and cysteine residues that bind to Zinc. A personalized zinc finger nuclease (ZFN) could be created for each patient’s specific mitochondrial mutation disease. The gene for this ZFN would be transmitted via a plasmid. Here is an illustration of how this could be done: 10. Cytoplasmic transfer (also called pro-nuclear transfer) – With inherited mitochondrial mutation disease, all of the mutant mitochondria come from the mother’s mitochondria (in the cytoplasm of the egg). A healthy egg donor with no mutant mitochondria could donate an egg. The nucleus of this egg would be removed from the healthy egg and the nucleus from the unhealthy (mother’s) egg implanted into the enucleated cell of the egg donor. This new egg would be fertilized by IVF methods and the child would be born with their father and mother’s nuclear DNA, but the mitochondria of the donor. This has already been done in Newcastle, UK. Here is an illustration of how this can be done: Cell Necrosis vs Apoptosis – Die fast (necrosis) or die slow (apoptosis): inner vs outer membrane Cells can die suddenly due to anoxia, mechanical crush injuries, etc. with no orderly death program. This is referred to as cell necrosis, and occurs in minutes to hours (Ex: heart attack or stroke). Necrosis is mediated by the mitochondrial permeability transition pore (MPTP) opening in the inner mitochondrial membrane, allowing rapid influx of water and solutes into the mitochondrial matrix. This has alreadybeen described in the section above. Apoptosis is different. It is a well-controlled, orderly series of steps that is programmed, takes 3-5 days to execute. Apoptosis is mediated by BAK or BAX, two pro-apoptic members of the Bcl-2 family which create holes in the outer mitochondrial membrane, allowing many triggers of apoptosis to pour into the cytoplasm (cytochrome c, SMAC, DIABLO, AIF, Endonuclease The illustration below from Kubli and Gustafsson’s article titled Mitochondria and Mitophagy: The Yin and Yang of Cell Death Control nicely illustrates the differences between necrosis and apoptosis. Cell Suicide (Intrinsic pathway of apoptosis) vs Cell Homicide (Extrinsic pathway of apoptosis) If apoptosis is triggered by the cell itself (suicide), this is called the intrinsic pathway of apoptosis. If the apoptosis is triggered by death signals (ligands) from outside the cell (homicide), this is called the extrinsic pathway of apoptosis. Apoptosis is part of normal embryology, fetal development, homeostasis, and old cell recycling. Between 50-70 billion cells die each day by apoptosis in the average adult. Orderly apoptosis produces no inflammation. Resistance to apoptosis is associated with cellular senescence in aging. Increased or decreased abnormal apoptosis is seen and in many degenerative, ischemic, and autoimmune disorders. With cancer, apoptotic pathways are defective and resistance to apoptosis by cancer stem cells are thought to be the cause of chemotherapy and radiation resistant cancers that re-occur. The entire apoptosis scheme is complex, the pathways are linked and also influence each other. Apoptosis can be self-inflicted (i.e. “suicide”) or caused by external forces (i.e. “homicide”) via death receptors. With cell necrosis, the plasma membrane ruptures, which produces an intense local inflammatory response. With apoptosis, there is no plasma membrane rupture. Instead, the contents of the cell are digested within the cell, then ingested by phagocytes that are attracted by released apoptotic bodies and/or the exposed phosphatidylserine residues that become exposed on the membrane surface as a result of the “phosphatidyl flip-flop” in late apoptosis. The “suicide pathways” are called the intrinsic pathway and are typically triggered by the loss of trophic factor binding to the cell surface receptors, by DNA damage, by excessive heat, misfolded proteins, severe hypoxia, high levels of ROS, chemotherapy, or viral infections. Regardless of the trigger, cell suicide is mediated by mitochondria. Cell “homicide pathways” make up the extrinsic pathway and are not triggered by mitochondira. Instead, they are triggered by “homicide proteins” (TNFα, TWEAK, Fas Ligand, APO3L, TRAIL, EDAL, NGF) via death receptors found on the plasma membrane. The extrinsic pathway will not be discussed much in this blog, since it is a non-mitochondrial death pathway, other than to mention that external sources of cell stress (heat, radiation, nutrient deprivation, hypoxia, viruses) still trigger cell suicide via the intrinsic pathway, not the extrinsic pathway. Even hormones like glucocorticoids which are clearly from external sources trigger apoptosis via the intrinsic pathway. For this reason, it is important that the reader understand that the terms “intrinsic” and “extrinsic” really refer to the pathway location and not the source location of cellular stress. Apoptosis has a third pathway called the Perforin/Granzyme pathway that is primarily an extrinsic-like pathway and has both caspace-dependent and caspace-independent components). The Perforin/Granzume pathway is primarily used by cytotoxic T cells and will not be discussed much in this blog as well, since it does not directly involved mitochondira. The extrinsic and intrinsic pathways are depicted in the following diagram from Favaloro’s 2012 paper titled the Role of Apoptosis in Disease. Merging of the Cascades – The Perforin/granzyme pathway, Intrinsic, and Extrinsic pathways merge. The extrinsic, intrinsic, and Perforin/granzyme pathways all merge to form a common “execution pathway”, called the Caspace cascade. The cascade is formed by a family of proteases called caspaces which are the “executioners”. Caspace 3 is the most important executioner in the pathway. Caspace cascade activation results in an ordered disruption of the cell without disruption of the plasma membrane, thereby preventing inflammation from occuring to surrounding tissues. The time line for complete apoptosis typically takes place over a period of several days and includes an ordered series of events. Early events are unique for each pathway and include apoptosome formation (intrinsic pathway), disc formation (extrinsic pathway), and perforin/granzyme entry into the cell via the mannose-6-phosphate receptor (Perforin/granzyme pathway). All pathways merge at the point of Caspace 3 activation and end up with the formation of membrane blebs which release small micelles called apoptotic bodies into the surrounding extracellular space. This is all well described in Susan Elmore’s recent review article from June, 2007 titled Apoptosis: A Review of Programmed Cell Death. Here is a diagram from her article: Mitochondrial mediated Apoptosis – Caspace-dependent and Caspace-independent pathways After ATP production, the most important function of mitochondrial may be their role in apoptosis. Although nuclear events can trigger apoptosis, apoptosis occurs normally in enucleated cells. Mitochondria trigger apoptosis by 2 methods: Caspace-dependent triggering (via cytochrome c, Caspace 9 directly, and by inhibiting the inhibitor, IAP) and Caspace-independent triggering (via ROS, EndoC, and AIF). Both of these mechanisms are part of the intrinsic pathway of apoptosis. These mechanisms are nicely diagramed in Jin and Reed’s article Yeast and Apoptosis from 2002, depicted below: 1. Caspace-dependent Mitochondrial Apoptosis – Cytochrome C triggering caspace cascade The most frequent triggers of the intrinsic pathway of apoptosis is unrepairable nuclear DNA damage. When this occurs, a protein ATM binds to the damaged DNA. ATM activates the master guardian of the genome, p53, which does many things including stopping cell division. Nuclear p53 triggers a protein Bax to migrate to the mitochondria where it forms pores in mitochondrial membranes, allowing the contents of the mitochondrial to “leak” out into the cytoplasm. One of the molecules that leaks out is Cytochrome C, which is an important trigger of the Caspace cascade. Cytochrome C binds to the adaptor protein, APAF, which then binds to inactive Caspace 9 (proCaspace). This complex activates Caspace 9 which then initiates a domino effect, activating more and more Caspace 9. Caspaces then destroy/degrade proteins, DNA, and most all molecules found within the cell. Intrinsic damage to mitochondria by ROS, or XRT also can trigger this Caspace-dependent mitochondrial mediated apoptosis. This sequence of events is illustrated in the of events is illustrated in the animation by Wagener and Muller. 2. Caspace-independent Mitochondrial Apoptosis – AIF, EndoC, and ROS triggering apoptosis Mitochondria can induce apoptosis without the help of the caspace cascade. These mechanisms are called caspace-independent pathways and are mediated by Apoptosis-inducing factor, EndoG, and ROS released by mitochondria. Apoptosis-inducing factor (AIF) is a protein normally found in the mitochondrial matrix, but migrates to the nucleus and triggers chromatin condensation and DNA degradation. Endonuclease G is a mitochondrial specific nuclease that also migrates to the nucleus to degrade DNA. Reactive oxygen species clearly play a role in apoptosis induction. ROS activated apoptosis is dependent on the activation of JNK and p38MAPK pathways in the cytosol. Mitochondria are both the primary source of ROS and the target of ROS in apoptosis. However, this appears toto degrade DNA. Reactive oxygen species clearly play a role in apoptosis induction. ROS activated apoptosis is dependent on the activation of JNK and p38MAPK pathways in the cytosol. Mitochondria are both the primary source of ROS and the target of ROS in apoptosis. However, this appears to be dose-dependent, since low ROS levels are anti-apoptotic (by activating Nrf2/ARE system), whereas high ROS levels are apoptotic (via JNK and p38MAPK pathways). 3. Mitochondrial suppressors of Inhibitors of Apoptosis (IAPs) – Smac/Diablo, Omi/HtrA2 Recently, a family of 8 proteins called inhibitors of apoptosis (IAPs) have been found that suppress apoptosis primarily via Caspace inhibition. These are up regulated in cancer. Most cancers also express a specific IAP called survivin, which is not expressed by normal cells. The list of IAPs keeps growing and includes such names as XIAP, clA +P1, clAP2, MLIAP, ILP2, NAIP, and survivin. When mitochondrial membranes are disrupted by Bax via the intrinsic pathway, they release two proteins, Smac/Diablo and Omi/HtrA2 which inhibit the IAPs. This “inhibition of inhibitors” results in the promotion of the Caspace dependent pathway. This is a 3rd mechanism how mitochondria increase apoptosis. The final feature of apoptosis sequence is the membrane “phospholipid flip-flop”of phosphatidylserine groups from the intra-cellular side of the plasma membrane to the extracellular side of the membrane. Both apoptotic bodies and the extracellular phosphatidylserine groups on the plasma membrane act as “eat me” signals for phagocytes to injest the dead cells before they rupture and cause inflammation. Mitochondria and The Balance of Life or Death–NF-kb and the TNF family double-edged swords Two different proteins were discovered in 1984 that killed cancer cells. For this reason, they were called tumor-necrosis factors (TNF). Today there are 19 members of the TNF superfamily that act as extracellular signaling molecules, binding to 29 cell surface receptors. The TNF ligands play a positive role in normal cell functions such as immune response, hematopoiesis and morphogenesis, but also are the mediators of many diseases such as tumorigenesis, transplant rejection, septic shock, viral replication, bone resorption, rheumatoid arthritis and diabetes, or cell death. The following diagram is an attempt to simplify this paradox and is from Van Horssen’s article titled TNF-α in Cancer Treatment: MolecularInsights, Antitumor Effects, and Clinical Utility. In all normal and cancer cells, life is a balance between survival proteins called anti-apoptotic factors (Ex: IAP, survivin, FLIP, XIAP, TRAP-1, BCL-XL) and death proteins called pro-apoptotic factors ( Ex: TNFR, FADD, Caspaces). Mitochondria do not play a significant role in TNF-mediated cell survival (other than the production of ROS, but play an important role in apoptosis via the pro-apoptotic Bcl-2 family members). Although the NF-kB transcription factor is often thought to be pro-apoptotic, it actually regulates eight anti-apoptotic factors. These include TRAP-1, the mitochondrial-specific Hsp90 chaperone discussed previously, and the inhibitors of apoptosis: IAP1, IAP2, survivin, FLIP, XIAP, DCR, and BCL-XL. Pro-apoptotic factors do not require active protein synthesis, but anti-apoptotic factors require active protein synthesis. The genes for anti-apoptotic factor synthesis are regulated by the transcription factor NF-kappaB. Although NF-kappaB is usually labeled as the “devil of inflammation”, NF-kappaB can also be viewed as the “savior of survival”. The following diagram from Aggarwal’s article titled Signalling pathways of the TNF superfamily: a double-edged sword nicely illustrates the balance of life and death by the TNF superfamily and clearly puts NF-kB on the “pro-life” side of the balance. Cancer and the Loss of Apoptotic Function – loss of normal apoptotic function is a hallmark of cancer
Cancer is typically thought of as a “loss of cell cycle regulation”, but research now clearly shows that a a loss of apoptotic function is of equal importance and is an early event in the sequential steps of carcinogenesis. Defects in “upstream triggers” of apoptosis (such as a defective p53 gene) are the most common cause of inadequate apoptosis in cancer. After “upstream mutations”, the most common apoptosis defects found in cancer include over-expression of the Bcl-2 family of proteins that are anti-apoptotic (Bcl-2). Less common mutations include apoptosome defects, death receptor pathway defects, and altered Caspace activity. Most cancers express survivin, which is an IAP that inhibits Caspace cascade at Caspace 7 and 9. IAPs can be induced by NF-kB, which explains why inflammation has been linked to tumor progression. Cancer therapies such as chemotherapy and radiation are typically given to induce apoptosis by damaging DNA, which triggers the mitochondrial-mediated intrinsic pathway. This strategy does not always work, however, and has major toxic side effects. The loss of apoptotic function in cancer cells is just one reason why chemotherapy and radiation do not always work. Non-toxic methods to induce apoptosis in Cancer Many non-DNA damaging strategies to attack cancer have been proposed. One idea is to reactivate apoptosis in cancer cells via an apoptotis pathway-specific manner. The advantage of this is that such a strategy could potentially be non-toxic, especially if the strategy only occurred in transformed or stressed cells. Some of the earliest work in this area involved the discovery that many phytochemicals found in nature would induce apoptosis. These compounds were found in herbs, teas, spices, and foods were investigated in vitro and in vivo. The most well-studied phytochemicals include curcumin, ECGC, resveratrol, fisetin, luteol, lycopene, lycopene, lupeol, and genistein. Today there is evidence that these compounds can induce apoptosis in cancer at multiple points in both the intrinsic and extrinsic pathways. Khan’s article reviews this well: Apoptosis by dietary agents for the prevention and treatment of cancer. The diagram below is from this article, showing where the compounds work.
There are many other strategies to induce apoptosis besides phytochemicals. Today there are over 1,000 clinical trials underway of non-DNA damaging apoptosis inducers for cancer. Most of these directly or indirectly involve mitochondria and this is why I am covering them in this article. Such strategies may someday be the key to aging, since senescent cells also have defective apoptotic pathways, like cancer. These nontoxic apoptotic strategies can be broadly classified into anticancer genes, Bcl-2 family protein inhibitors of anti-apoptotic members, IAP inhibition, death receptor pathway activation, and both NF-kB inhibition and NF-kB activation. Other indirect strategies such as immune therapy, triggering the UPR pathway, etc. will not be covered here, but will be covered in future blogs on those subjects. 1. Anticancer genes – Apoptin, Brevinin 2R, E4orf4, HAMLET, Mda-7, Noxa, NS1, ORCTL3, TRAIL Anticancer genes are genes that code for small polypeptides than specifically harm cancer cells but do not harm normal cells. These proteins induce either autophagic cell death or apoptotic cell death only in cancer cells. They are completely nontoxic in noncancer cells. Many of these genes were found in viruses. Others are proteins found in milk. There is a good review of this in Grimm and Noteborn’s recent article. This diagram below is from their article. Phase I and II clinical trials are already underway for TRAIL, Mda-7, and HAMLET. 2. Bcl-2 family anti-apoptotic factor inhibition – Genasense, Gossypol, Polyphenol E, GX-15-070, HA14-1 analogs, ABT-737, Apogossypol, BH3I-1/BH3-1-2, Antimycin A3, Terphenyl derivative. There are six proteins in the human family of Bcl-2 family that are antiapoptotic. (Bcl-2, Bcl-Xl, Bcl-W, Bfl-1, Bcl-B, and Mcl-1). Many cancers overexpress one or two of these, accounting for their chemoresistance. Antiestrogens (tamoxifen) and retinoids (retinoic acid) suppress BCL2 gene expression via the nuclear receptor at the gene promoter site, but the results of these drugs on inhibiting apoptosis is unpredictable. For this reason, several specific agents are in development by pharmaceutical industry and at academic labs (see list above). These include anti-sense oligonucleotides (Genasense) against BCL2 mRNA which has already entered Phase III trials. Many natural compounds also antagonize Bcl-2 by binding to the BH3-binding site on Bcl-2. This includes gossypol (from cotton seeds), EGCG (from green tea), theaflavins (from black tea), Cherythrine (from tropical plants), and antimycin A (from bacteria) which bind to Bcl-2 and Bcl-XL at 0.1 to 10 μM concentrations. These natural compounds are currently being tested in preclinical and Phase I studies at the Mayo Clinic, NCI, Yale University, and many other academic labs. Synthetic analogs are also being studied by Abbot Labs and Gemin X. 3. IAP inhibition – employing XIAP antisense, survivin antisense, peptides, embelin, Di/Triphenylureas, Compound 3. The IAP family of proteins directly bind to caspases and block apoptosis. The Caspaces 3, 7, and 9 are the primary ones blocked by IAPs. Studies suggest that cancer cells are more dependent on IAPs than normal cells, and IAP inhibitor studies show far do not show toxicity in normal cells. Antisense oligonucleotides against IAP mRNA have already entered Phase I studies (XIAP antisense, surviving antisense). Two other strategies have been developed for IAP inhibitor discovery: 1) mimicking endogenous IAP inhibitors (smac/Diablo, omni/HtrA2) or 2) high through-put caspace enzyme assays. Embelin is a natural IAP inhibitor found in traditional herbal medicines for cancer. It has been found to enhance the therapeutic efficacy of radiation for prostate cancer in preclinical studies. 4. TRAIL. The TNF super family has 19 known members and they can induce apoptosis via mitochondrial and mitochondrial-independent pathways. They include TNFα, Fas Ligand (FasL), and TNF-related apoptosis-inducing Ligand (TRAIL). Unfortunately, TNFα is highly toxic since it produces intense inflammation. TNFα also induces NF-kB pathway, which induces multiple antiapoptosis pathways (see discussion above). For this reason, TNFα is not a good candidate for inducing apoptosis. The TRAIL cytokine can induce apoptosis without causing inflammation. A soluble form of TRAIL is nontoxic to normal cells but shows promising efficacy in preclinical studies. A Phase I trial of TRAIL has already been initiated and an antibodies against the TRAIL receptors have already entered Phase II studies. These are well tolerated without toxicity, but determining what cancers will respond to death receptors is empiric science right now, and very unpredictable from case-to-case. One reason for the unpredictable TRAIL response is the c-FLIP protein, an intracellular protein overproduced by cancer cells that suppresses signals from death receptors. Several strategies have been developed to reduce c-FLIP. Another strategy is to downregulate TRAIL inhibitors (c-FLIP, c-FLIPL, and c-FLIPS) by the cancer, to induce apoptosis by an autocine feedback mechanism. A compound called flavopiridol, a flavone derived from a natural compound called rohitukine, found in the bark of a plant from India, has been found enhance TRAIL-induce apoptosis by downregulating TRAIL inhibitors. Flavopiridol has already undergone Phase II clinical trials, but did not show any effect in a Phase II trial of non-small cell lung cancer. Another natural compound found in vanilla, vanillin, has been shown to selectively kill cancer cells with little effect on normal cells. Pre-treatment of with Vanillin has been shown to kill TRAIL-resistant human cervical cancer cells by prevention of NF-kB activation. This mechanism will be discussed in the section below. 5. The NF-kB pathway and its “Jekyll and Hyde” behaviour in cancer apoptosis The NF-kB pathway is a family 5 genes that gives rise to 7 proteins that share a Rel Homology domain. (NF-kB1, NF-kB2, RelA, c-Rel, and RelB). These proteins are held in the cytoplasm by their interaction with IkB proteins. When pro-inflammatory cytokines or viral infections occur, the IkB proteins are phosphorylated and then undergo ubiquitination and degradation by the proteasome. This allows the NF-kB proteins to translocate to the nucleus where they function as transcription factors. In normal cells, activation of the NF-kB pathway is inducible and produces a transient response. In cancer cells, NF-kB looses its “inducibiliby” and remains “activated” continuously. This leads to dysregulation of all of the genes that NF-kB normally turns on, resulting in continuous over-expression of these genes. This includes genes that prevent apoptosis by both mitochondrial (intrinsic pathway) and death receptor (extrinsic) pathways. The genes include FLIP (TRAIL inhibitor), which prevents Caspace binding to the Death-Inducing Signaling Complex (DISC), blocking the extrinsic pathway. NF-kB also induces gene expression Inhibitors of Apoptosis (IAPs) well as genes for anti-apoptotic members of the Bcl-2 family. NF-kB even down regulates p53, the “master on switch” for apoptosis. As a result of all these in vitro studies of NF-kB activation, NF-kB became a very popular idea for preventing cancer and treating cancer. This let to reports using many naturally ocuring phytochemicals to inhibit the NF-kB pathway. These studies included genistein (soybeans), isothiocyanates (broccoli, brussel sprouts), curcumin (turmeric), and many other polyphenols. Despite very good data in vitro and in vivo in the laboratory, these compounds were mostly not used alone in clinical trials, but were combined with chemotherapy or radiation therapy to enhance apoptosis. Unfortunately, some studies showed no efficacy and further laboratory studies have supported the fact that NF-kB inhibition can be pro-apoptotic in some cancers and NF-kB activation is pro-apoptotic in other cancers. The keys to understanding the “good cop-bad cop” role of NF-kB include the following 3 discoveries: 1) The 7 NF-kB proteins activate different gene profiles. 2). phosphorylation of the p65 subunit of NF-kB proteins is critical to transcription factor activity, and 3) NF-kB has a crtical pro-apoptotic role in p73-dependent cell death, whereas NF-kb as an anti-apoptotic role in p53-dependent cell death. and 3) NF-kB has a crtical pro-apoptotic role in p73-dependent cell death, whereas NF-kb as an anti-apoptotic role in p53-dependent cell death. Cellular Senescence and Apoptosis Resistance – apoptosis resistance is a hallmark of senescence As discussed in the previous section, cancer cells loose cell cycle control due to different genetic mutations. In approximately 50% of human cancers, p53 is mutated or silenced, accounting for both the loss of cell cycle control and the loss of normal apoptosis. With cellular senescence, however, p53 works fine and is up regulated along with p16. These two upregulated cell cycle checkpoint proteins account for the irreversible cell cycle arrest seen in cellular senescence. In this aspect, cancer and senescence are opposites. Initially, the trigger for p53-driven cell cycle arrest was thought to be solely caused by telomere shortening during each round of DNA replication, with the cells reaching the “Hayflick limit” after 50-60 cell divisions. Later it was found that senescent cells can undergo p53-driven and/or p16 driven cell cycle arrest without telomere shortening. Many factors account for this paradox. For instance, oxidative stress, psychologic stress, CMV infection, and many diseases will accelerate telomere shortening independent of cell division or telomerase activity. Exercise, fish oil, estrogen, caloric restriction, and many phytochemicals delay telomere shortening independent of cell division or telomerase activity. Although proprietary supplements have been shown to delay mean telomere length shortening in non-randomized studies, no randomized clinical trials of these supplements have been shown to prevent disease, reverse disease, prevent aging, or reverse aging. As a result, telomere length may not be as good of a biomarker for aging or disease as was originally thought. For an more extensive review of this topic, please refer to Vince Giuliano’s blog from May, 2012 entitled Telomerase update – arguments for and against using telomere extender supplements. Today, most scientists have shifted this discussion to the broader subject of cellular senescence, rather than just focusing on telomere length. We now know there are many causes of cellular senescence besides telomere shortening. As a result, cellular senescence is now classified into subcategories by the cause of cell cycle arrest: (telomere-dependent senescence, DNA damage-induced senescence, oncogene-induced senescence, senescence caused by chromatin perturbation, and ROS-induced senescence, and stress-induced senescence, etc.) Paradoxically, both cancer and senescent cells exhibit resistance to apoptosis.. As a result, senescent cells are very stable in cell culture but will not divide. Unlike cancer, the apoptosis resistance seen with cellular senescence is not universal. The apoptosis resistance is also cell-specific, trigger-specific, and dependent onthe point in the cell cycle where the arrest occurred. For example, senescent fibroblasts are resistant to ceramide-induced apoptosis, but endothelial cells are not. . Senescent fibroblasts are also resistant to intrinsic pathway apoptosis by growth factor deprivation or oxidative stress, but are still sensitive to extrinsic pathway apoptosis by Fas death receptor activation. Cause of Apoptosis Resistance in Senescent Cells – Failure of IGFBP-3 re-uptake by endocytosis The cause of apoptosis resistance in senescent cells is not as well known as it is in cancer cells. One study has suggest that defects in the endocytotic re-uptake of IGF binding protein 3 (IGFBP-3) is the cause of apoptosis resistance. A thorough discussion of the six IGF binding proteins has been recently published by Firth and Baxter. The major function of IGFBP-3 is to sequester IGF, modulating its binding to the IGF receptor. IGFBP-3 is normally secreted out of the cell and binds to extracellular IGF-1. By this mechanism, low concentrations of extracellular IGFBP-3 block survival signals (via AKT signaling). With high concentrations of extracellular IGFBP-3, a completely different effect occurs (in normal cells). High extracellular concentrations of IGFBP-3 trigger re-uptake of the extracellular IGFBP-3 by endocytosis. This phenomena is independent of IGF-1 levels. Once inside the cell, the IGFBP-3 translocates to the nucleus where it induces intrinsic pathway apoptosis via bax, even in the absence of a functional p53. Here is a diagram from Wick’s article A Darwinian-evolutionary concept of age-related diseases.
In senescent cells, IGFBP-3 re-uptake by endocytosis does not occur. Hampel et al showed that in human fibroblasts, the degree of apoptosis resistance correlated well with the absence of nuclear IGFBP-3. In these senescent cells, IGFBP-3 is highly overexpressed and was effectively secreted out of the cell. The conditioned media of these fibroblasts had high levels of IGFBP-3 but none of the protein was endocytosed or transported to the nucleus. As a result, the low levels of nuclear IGFBP-3 caused apoptosis resistance. Conclusion: Cancer and senescent cells are apoptosis resistant, but the mechanisms of resistance are very different. In the case of cancer, the most common cause is a mutated p53, but many other mutations of apoptotic factors or overexpression of anti-apoptotic factors occurs. In addition, unique IAPs such as survivin are up regulated with cancer. Unlike cancer, p53 is functional and up regulated in senescent cells, along with the p16-Rb pathway. In one study, a defect in IGFBP-3 re-uptake by the senescent cell leads to a lack of nuclear localization of IGFBP-3. This resulted in apoptosis resistance. Naturally occurring phytochemicals such as isoflavanoids, curcuminoids, isoflavones, have have been shown to induce apoptosis at multiple points in both intrinsic and extrinsic pathways of apoptosis. To date, no study has shown that these phytochemicals will induce apoptosis in senescent cells, however. Since p53 is functional and activated in senescence cells, p53-dependent apoptotic pathways should be enhanced by NF-kB inhibitors with much more reliability than the “Jekyll and Hyde” effect of NF-kB inhibitors in cancer. Inducing nontoxic, selective apoptosis in senescent cells without the need for gene therapy would be a wonderful treatment for aging, if such a compound/effect could be found. The two histologic hallmarks of AD are extracellular Amyloid–β plaques and neurofibrillary tangles inside neurons. Amyloid-β aggregates because the Amyloid Precursor Protein (APP) is cleaved in the wrong place by β-secretase (rather than correct cleavage by alpha-secretase). This “scissor mis-snip” occurs just before the amyloid peptide is secreted into the extracellular space. As a result, The 40 and 42-amino acid long fragments aggregate into Amyloid-beta plaques and create severe inflammation. A-β40 is much more common, but A-β42 is much more neurotoxic, causing neuronal cell death. The appearance of A–β plaques precedes the 2nd hallmark finding in AD: intracellular neurofibrillary tangles (NFT). NFT occur due to the breakdown of microtubules, which stops axoplasmic transport and the loss of cytoskeletal stability. NFT occurs in association with the accumulation of intracellular tau protein aggregates. The tau proteins in NFTs are hyperphosphorylated in AD. Amyloid aggregates are broken down by proteases (including caspaces) and apolipoprotein E (ApoE) facilitates this. The ApoE4 version of this protein is not an efficient catalyst of this reaction. Activated caspace breaks down A-β and A-β triggers Caspace 3 activation. Caspace 3 can also create A-β by cleaving APP. This means that the Caspace pathway of apoptosis plays a role in both the cause and the effect of AD. The caspace pathway also plays a role in NFT clearance – Tau protein is a substrate for Caspace 3. The evidence that the caspace pathway plays a causal role in AD was further strengthened in animal studies where over-expression of anti-apoptotic proteins such as Bcl-2 inhibited the formation of A–β plaques, tau neurofibrillary tangles, and improved memory. For this reason, more focus on the role of apoptosis in AD should be made. Many treatments for Alzheimer’s disease have been proposed, including anti-cholinesterase inhibitors, antibodies against A-β, Copper ions, SOD, GSH, Mifepristone, Tacrine, MAEHP, D-penicillammine, Rivastigmine, EGCG, and Ferrulic acid. Five drugs are approved by the US FDA for AD. Four are acetylcholinesterase inhibitors (galantamine, rivastigmine, donzepil, tacrine) and one is an antagonist of NMDA (memantine). None of these drugs treat the cause or stop the progression of the disease. Three large Phase III clinical trials of anti- A-β antibodies were halted in 2012, since they failed to show efficacy, even in homozygous ApoE4 patients. None of these are inhibitors of apoptotic pathways. Paradoxically, curcumin and EGCG have been shown in experimental transgenic mouse models of AD to inhibit apoptosis. This is the opposite of their apoptotic effects on cancer. Here is a diagram of the chemical structures of these compounds: Apoptosis in Alzheimer’s disease (AD) –neuronal apoptosis due to “miss-snipping” of amyloid precursor protein Alzheimer’s disease (AD) is the most common neurodegenerative disease and affects 10% of the population over 65 years of age. Familial AD only accounts for 2-3% of AD cases and the rest are sporadic, but 14% of the US population carries the single nucleotide polymorphism for the ApoE4 allele, which increases the risk of AD by 10-30 fold if the person is homozygous for the ApoE4 allele. The causal relationship between ApoE4 status and the development of the disease is still in question, since a 1/3rd of the patients who develop AD are ApoE4 negative. ApoE proteins are thought to enhance proteolytic breakdown of Amyloid-β- plaques and the ApoE4 form is not as efficient at catalyzing amyloid-β? breakdown. What is clear, however, is that neuronal apoptosis is the cause of memory loss in AD, and this may explain why so many strategies to reverse memory loss with AD have failed. (You can’t bring dead neurons back to life!) The intrinsic pathway of apoptosis initiated by mitochondria appears to be the primary pathway activated in AD. The triggers for intrinsic pathway activation in AD are poorly understood, but are thought to be amyloid-β, inflammation, and proteins from microtubule breakdown called tau. The two histologic hallmarks of AD are extracellular A-β plaques and neurofibrillary tangles inside neurons. Amyloid-β aggregates because the Amyloid Precursor Protein (APP) is cleaved in the wrong place by β-secretase (rather than correct cleavage by ?-secretase). This “scissor mis-snip” occurs just before the amyloid peptide is secreted into the extracellular space. As a result, The 40 and 42-amino acid long fragments aggregate into Amyloid-? plaques and create severe inflammation. A-?40 is much more common, but A-?42 is much more neurotoxic, causing neuronal cell death. The appearance of A-? plaques precedes the 2nd hallmark finding in AD: intracellular neurofibrillary tangles (NFT). NFT occur due to the breakdown of microtubules, which stops axoplasmic transport and the loss of cytoskeletal stability. NFT occurs in association with the accumulation of intracellular tau protein aggregates. The tau proteins in NFTs are hyperphosphorylated in AD. Amyloid aggregates are broken down by proteases (including caspaces) and apolipoprotein E (ApoE) facilitates this. The ApoE4 version of this protein is not an efficient catalyst of this reaction. Activated caspace breaks down A-? and A-? triggers Caspace 3 activation. Caspace 3 can also create A-? by cleaving APP. This means that the Caspace pathway of apoptosis plays a role in both the cause and the effect of AD. The caspace pathway also plays a role in NFT clearance – Tau protein is a substrate for Caspace 3. The evidence that the caspace pathway plays a causal role in AD was further strengthened in animal studies where Over-expression of anti-apoptotic proteins such as Bcl-2 inhibited the formation of A-? plaques, tau neurofibrillary tangles, and improved memory. For this reason, more focus on the role of apoptosis in AD should be made. Many treatments for Alzheimer’s disease have been proposed, including anti-cholinesterase inhibitors, antibodies against A-?, Copper ions, SOD, GSH, Mifepristone, Tacrine, MAEHP, D-penicillammine, Rivastigmine, EGCG, and Ferrulic acid. Five drugs are approved by the US FDA for AD. Four are acetylcholinesterase inhibitors (galantamine, rivastigmine, donzepil, tacrine) and one is an antagonist of NMDA (memantine). None of these drugs treat the cause or stop the progression of the disease. Three large Phase III clinical trials of anti-A-? antibodies were halted in 2012, since they failed to show efficacy, even in homozygous ApoE4 patients. None of these are inhibitors of apoptotic pathways. Paradoxically, curcumin and EGCG have been shown in experimental transgenic mouse models of AD to inhibit apoptosis. This is the opposite of their apoptotic effects on cancer. Here is a diagram of the chemical structures of these compounds:
Curcumin and the failure of clinical trials for AD Curcumin is the most studied natural phytochemical for the treatment of AD. Although the mechanism of action of curcumin in cancer is by the induction of apoptosis; this does not appear to be the mechanism of action in AD. Instead, curcumin works via multiple other mechanisms. These are well described in Mishra’s article The effect of curcumin (turmeric) on Alzheimer’s disease: an overview. The following diagram illustrates these pathways: A recent randomized, placebo-controlled study from UCLA, of 36 patients with mild to moderate AD was published in October, 2012. They used an oral dose of 2g/day and 4g/day (vs placebo) for 24 weeks. The results showed no differences in treatment groups, although it was noted that plasma curcumin levels were low in the 2 and 4gm/day groups (7.32 ng/dl), due to poor absorption and bioavailability. 21% of patients the treatment group withdrew due to GI side effects, prompting some researchers to condemn the use of curcumin for AD. advantage of the ApoE transport system to improve transport across the blood brain barrier by creating drug-laden nanoparticles coated with the ApoE protein. Improving Curcumin with Nanotechnology The absorption, bioavailability, and side effect problems has prompted many to propose nanoparticle delivery forms of curcumin and other AD drugs. A review of this idea has been written by Brambilla et al. One of the novel ideas is to take advantage of the ApoE transport system to improve transport across the blood brain barrier by creating drug-laden nanoparticles coated with the ApoE protein. Here is a diagram illustrating this idea:
Conclusion: The etiololgy of AD is still unknown, but neuronal apoptosis is the cause of memory loss. Current FDA approved drugs are directed at preventing acetylcholine breakdown, but do not affect the natural history of memory decline or progression of other symptoms. With the failure of amyloid-clearing strategies such as antibodies against A-? and the failure of curcumin trials as well, it is time to reconsider the role of mitochondrially mediated, caspace-dependent apoptosis in the pathogenesis of the disease. Nanotechnology solutions may solve the absorption, bioavailability, and increase BBB penetration. Apoptosis in Parkinson’s disease (PD) – neuronal apoptosis of dopaminergic neurons due to misfolded ?-synuclein The hallmark of PD is a “dopaminergic neuron-specific apoptosis in the midbrain substantia nigra. Tragically, the 1st signs and symptoms occur only after 70% of the dopaminergic neurons are dead! Emerging evidence from the study of inherited forms of PD point to gene mutations in mitochondrial nuclear genes (such the study of inherited forms of PD point to gene mutations in mitochondrial nuclear genes (such as parkin, DJ-1, PINK1, etc.). A normal PINK1 gene inhibits mitochondrial-dependent intrinsic apoptosis. However, other studies have shown involvement of the non–mitochondrial extrinsic pathway as well. There is evidence that curcumin has a potential therapeutic role for Parkinson’s disease. Many other natural products may exert beneficial effects via similar mechanisms and are well described by effects via similar mechanisms and are well described by Mythri in a recent review article. Huntington disease (HD) – neuronal apoptosis of the striatum and cortex due to misfolded Huntington protein Huntington’s disease is part of a family of trinucleotide repeat diseases where the CAG repeat is expanded in the Huntington protein gene, resulting in protein misfolding and intracellular protein aggregates in the striatal and cortical neurons. Caspace 6 cleavage of the misfolded Huntington protein is required for the clearance of the Huntington protein from cells. Mitochondrial Heat Shock Response (the chaperonins)– the bidirectional “protein traffickers” between the cell and the mitochondria and their role as key stress signalers Once thought to only function as protein folders, today the consensus is that heat shock molecules are some of the earliest signaling molecules to evolve within prokaryotic cells. The heat shock response has a much longer half life than the ROS-response pathways described in the next section, which appear to be very “fast acting”, but also much more transient in duration. Heat Shock proteins are found in the mitochondrial during non-stressed, baseline conditions, but their expressions is dramatically up regulated by three conditions: 1) physiological conditions (cell cycle division, growth factors, cell differentiation, etc.), 2) pathological conditions (viral, bacterial, and parasitic infections, fever, inflammation, ischemia, hypertrophy, oxidant injury, cancer, autoimmunity), and 3) environmental factors (heat, heavy metals, metabolic inhibitors, amino acid analogs, ethanol, antibiotics, and radiation). The heat shock proteins can be subclassified into ATP-dependent and ATP-independent HSPs. (The larger ones are ATP dependent and the smaller ones are ATP-independent). HSPs can also be classified into 3 functional groups, as follows: 1. HSPs expressed in baseline, unstressed cells – Hsp-60, Hsp-70, Hsp-90, Hsp-110 The primary role of these Hsps is protein folding, also referred to as a “molecular chaperone.”. These HSPs are all ATP-dependet. The mitochondrial HSP60 is a member of this family. 2. HSPs expressed with glucose deprivation – Grp-34, Grp-47, Grp-56, Grp-75, Grp-78, Grp-94 These heat shock proteins also are molecular chaperones and include the mitochondrial Hsp, Grp-75 (also known as mt-Hsp70). 3. Small molecular weight HSPs – Hsp-10, Hsp-20, Ubiquitin These heat shock proteins regulate the actin cytoskeleton (Hsp20), are involved in the nonlysosomal protein degradation (Ubiquitin), or help Hsp60 (Hsp-10)
|

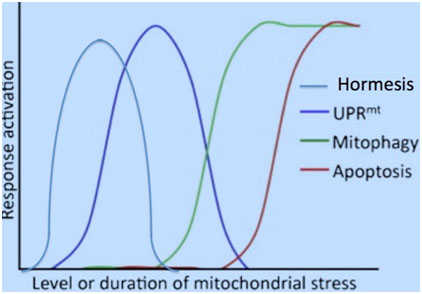
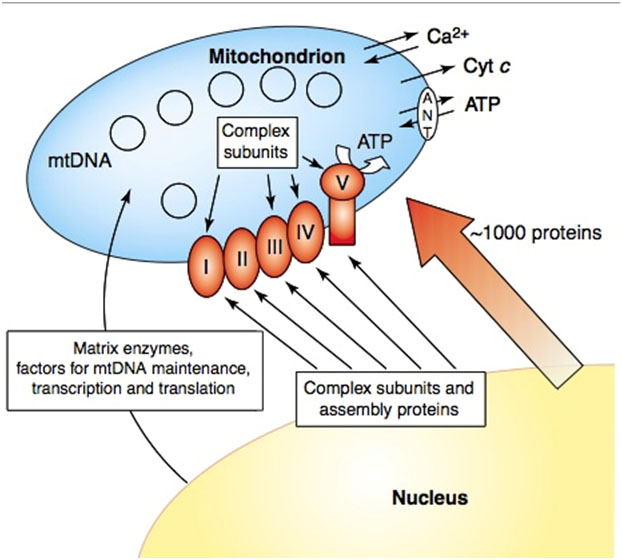
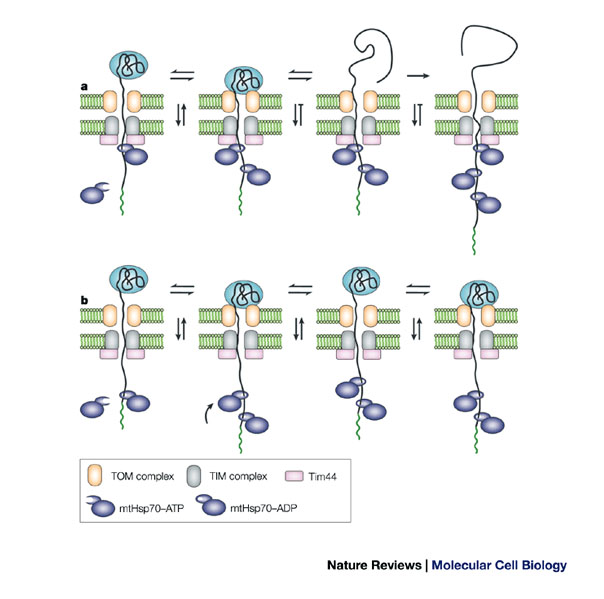
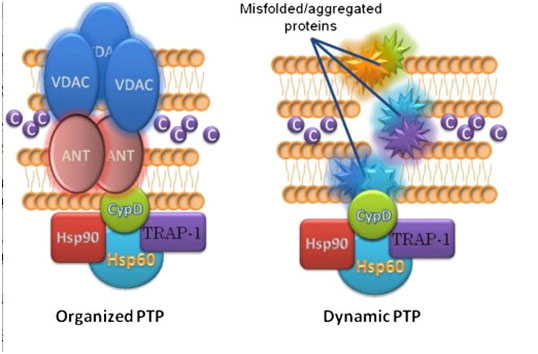
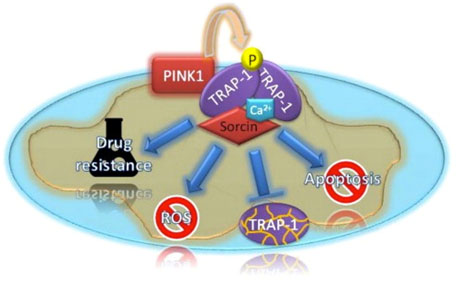

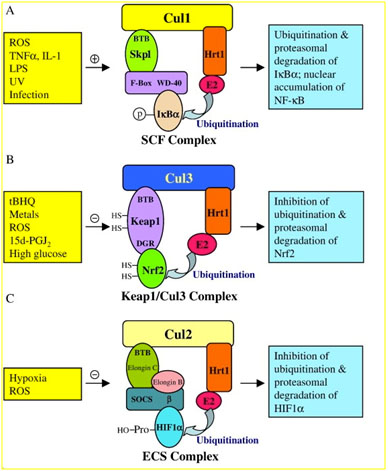


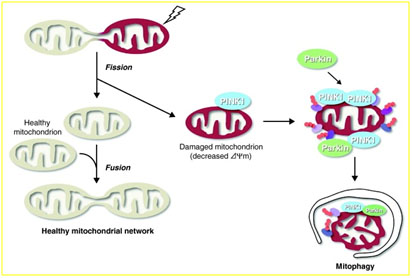
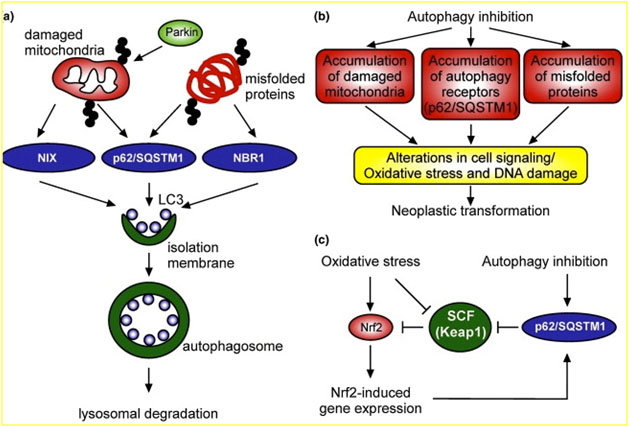
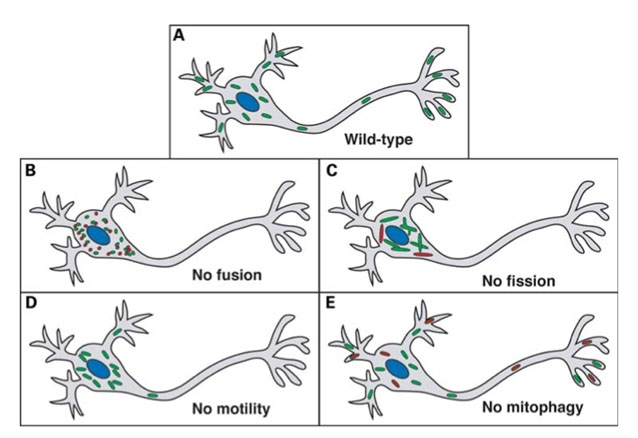
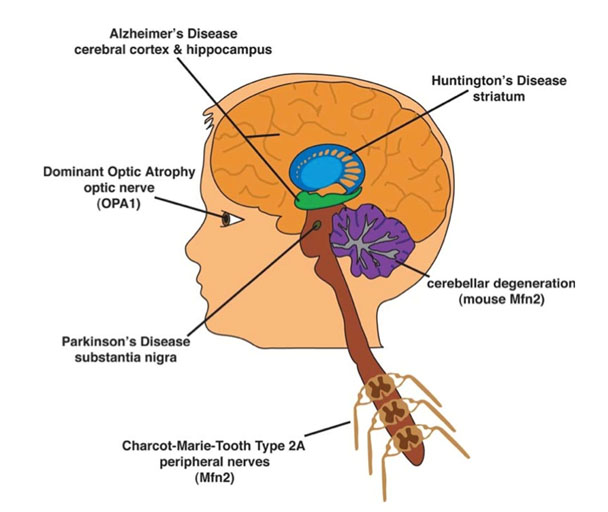
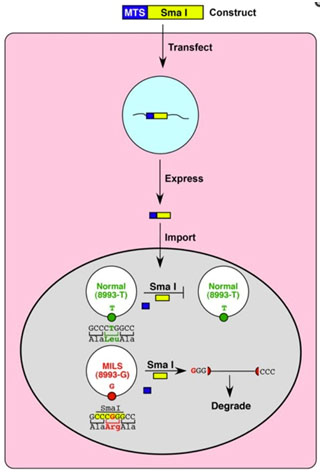


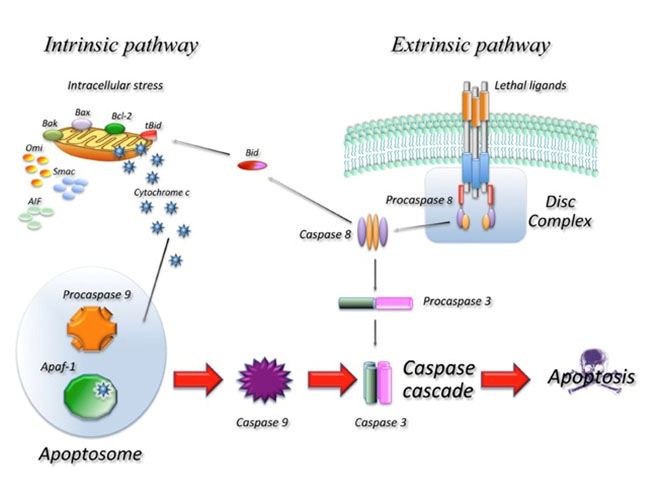
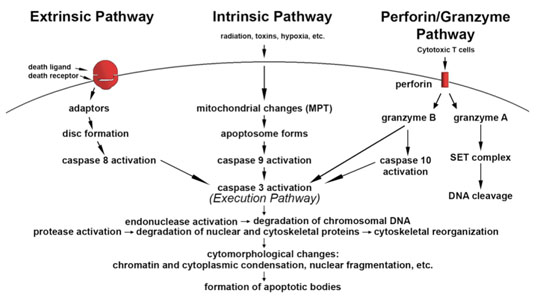
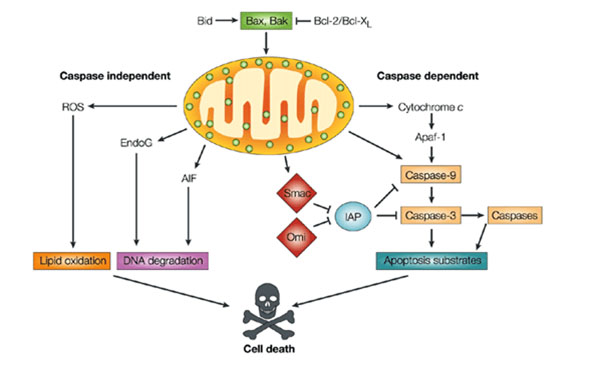
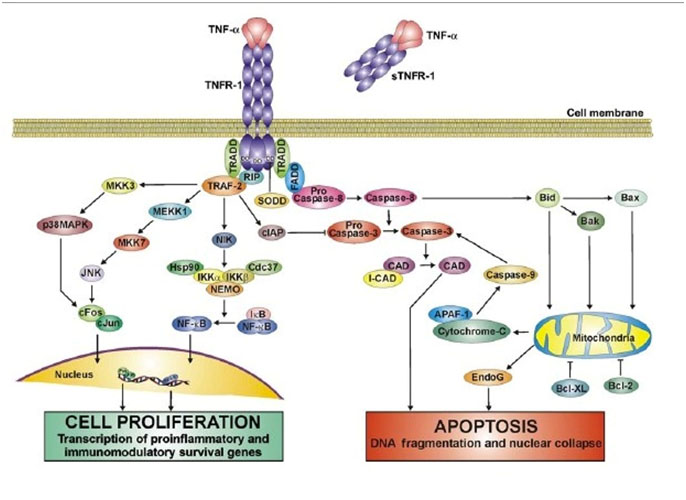
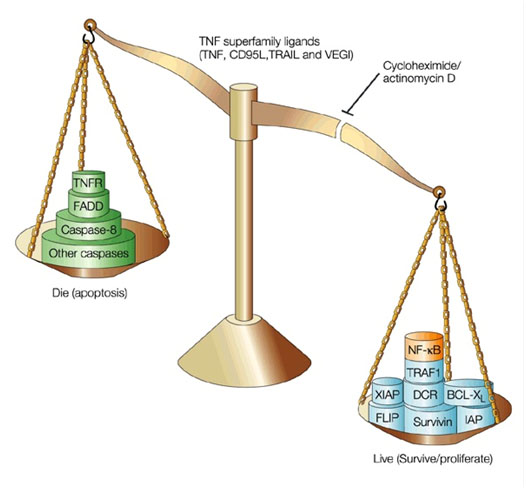
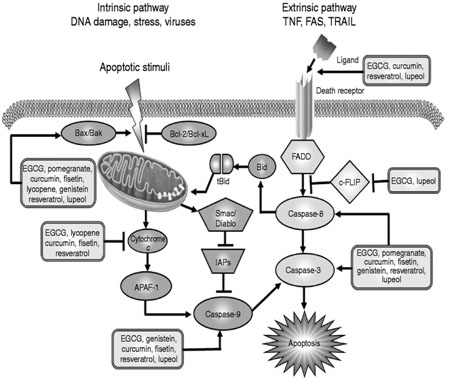
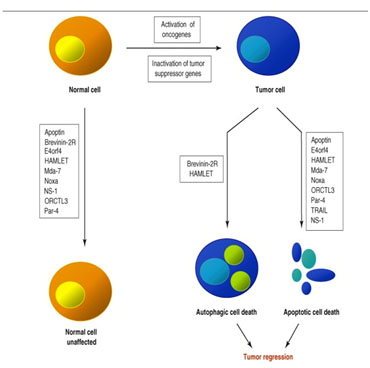
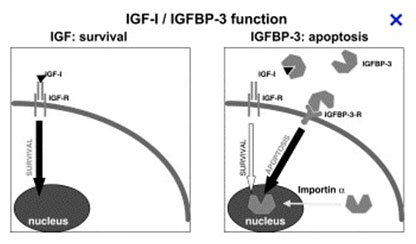
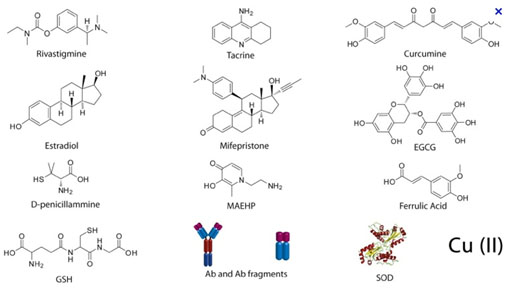

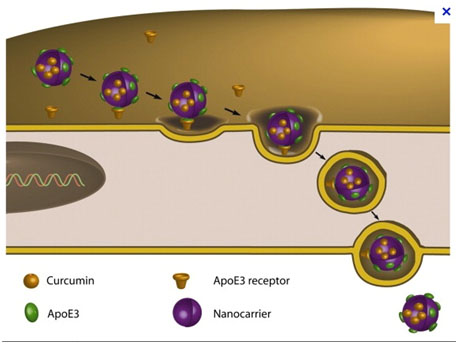

Pingback: Heat Shock Proteins and the Brain: Implications for Neurodegenerative Diseases and Neuroprotection · My-infoWorld.NET
Vincent
Just reading an interesting article about given nitric oxide producing bacteria to C. Elegans to increase life span. I wonder if the same bacteria or a close relative could be feed or given via enema to animals to increase lifespan? Maybe feed the C Elecans and then we or an anomal gets the C Elegans as food or the other way as an enema?
Eric
Nitric Oxide: A Little Molecule’s Remarkable Feat — Prolonging Life, Worm Study Shows
http://www.sciencedaily.com/releases/2013/02/130214132623.htm
Here is the link to the journal article ==>
Ivan Gusarov, Laurent Gautier, Olga Smolentseva, Ilya Shamovsky, Svetlana Eremina, Alexander Mironov, Evgeny Nudler. Bacterial Nitric Oxide Extends the Lifespan of C. elegans. 14 February 2013, Cell DOI: 10.1016/j.cell.2012.12.043
eric25001:
Thanks for the interesting link. What is reported seems to be yet-another example of life extension in lower species via a hormetic stress-induced process, this time interestingly via ingestion of a bacteria that produces NOS. “What we found is that nitric oxide gas produced in bacteria inside the worms diffuses into the worm tissue and activates a very specific set of genes acting through two master regulators, hsf-1 and daf-16, resulting in a high resistance to stress and a longer life.” HSF1 is a heat shock protein activated by the stress induced by the NOS. A number of other stress interventions also increase the lives of C. Elegans, and a number of other stresses in humans upgrade the expression of NOS.
Vince
Pingback: Autophagy – the housekeeper in every cell that fights aging | AGING SCIENCES – Anti-Aging Firewalls
Pingback: THE HORMESIS BARS | AGING SCIENCES – Anti-Aging Firewalls
Pingback: Glucosamine for longevity | AGING SCIENCES – Anti-Aging Firewalls