By James P Watson, with editorial assistance and comments by Vince Giuliano and Melody Winnig
Initial comments – by Vince Giuliano
This blog entry is about thoroughly documented health and possible longevity benefits of meditation, quite apart from possible spiritual benefits and largely independent of the various disciplinary approaches to meditation. The content is supported by many studies with over 130 research citations listed here. The content is also very closely related to the topics treated in of a number of other recent blog entries. These together begin to piece together both a theoretical basis for health and longevity and a highly practical agenda for achieving it. Namely:
- 1. Management of constitutional stress is one of the primary aspects of health that meditation is good for. A number of recent blog entries have focused on the use of wearable techology for day-to-day monitoring of constitutional stress and identifying what personal lifestyle patterns are most and least helpful in this regard. See the blog entries in the Digital Health series: Part 1 Digital health – health and fitness wearables, apps and platforms – implications for assessing health and longevity interventions, Part 2: looking for practical stress biomarkers, Part 3: Heart Rate Variability: Principles and Science and Practical Measuring Devices and Part 4: Heart rate stress biomarkers derivable from smart watch data. Combining meditation and personal stress monitoring could be a powerful personal approach to health.
- Management of key metabolic factors related to health. Meditation up-regulates SIRT1 gene expression and has a number of positive effects on basic metabolic pathways affecting DNA repair, mitochodrial health, and telomere lengths, Readers of this blog will recognize that we have discussed these and closely related topics in depth, I mention only a few of the most-recent blog relevant entries from the series NAD+ an emerging framework for health and life extension — Part 1: The NAD World, Part 2: Deeper into the NAD World, hopeful interventions, Part 3: 30 Major Factors that Control SIRT1 Expression, SIRT1 Activity, and SIRT1-mediated Aging. and Part 4:the NQ01 gene, the Warburg effect, SIRT 1 and inflammation, and possible interventions. Meditation is a worthy addition to the health interventions mentioned in these blog entries.
- Maintenance of mental balance, positive outlook and averting dementias. Meditation does these things, remarkably well. We published the blog entry A simple, comprehensive plan to prevent or reverse Alzheimer’s Disease and other neurodegenerative diseases – Part 1: The Plan. To that plan we add meditation.
- Discussions of basic pathways involving chronic stresses, inflammatory processes and healthful interventions. Meditation reduces stress and contributes to controlling inflammation. Nrf2 and NF-kappaB have long been featured in this blog as well as the benefits of xenohormetic interventions involving phytochemicals – far too many links to list here but they can be found by searching in the blog.
- 5. Roles of circadian rhythms, sleep and sleep stages and relationship of sleep stages to what occurs in meditation Meditation must work via established evolutionarily-driven biological mechanisms. Most likely, these are mechanisms that are encountered in sleep, REM sleep in particular, and have to do with balance of control between the sympathetic and parasympathetic nervous systems. We have touched on these topics in a number of blog entries. For example, the physiologic mechanisms described in the Part 3: Heart Rate Variability entry are possibly key for explaining what goes on in meditation as suggested by the final study described here.
Brief history of meditation – by Melody Winnig
Archeologists and scholars speculate that primitive hunter-gatherer societies may have discovered meditation and its altered states of consciousness while staring at the flames of their fires, although there is little recorded pre-history on the origins of meditation. Meditation as a systematic practice gradually evolved in India and China.
The earliest documented records of meditation stem from the teachings of the Vedas in ancient India, about 1500 BCE. Around the 6th to 5th centuries BCE, other forms of meditation developed in Taoist China and Buddhist India. Buddha lived from about 563 BC to about 483 BC and taught in Sarnath, India. Early written records of the multiple levels and states of meditation in Buddhism in India are found in the sutras of the Pāli Canon, which dates to 1st century BCE. By 653 CE The first meditation hall opened in Japan and Japanese Buddhism and began to evolve in the 8th century.
Although for many centuries mediation was primarily only practiced in Asia, Christian, Jewish and Muslim mystics each developed their own forms of meditative practices. By the 18th century translations of ancient eastern teachings began to be studied by scholars in the West.
But it wasn’t until the late 1950’s that non-Asian immigrants in the West began delving into meditation, particularly Zen which was in part popularized by the beat poets Alan Ginsburg, Jack Kerouac and Gary Snyder and writers such as Alan Watts, Philip Kapleau and D. T. Suzuki.
In 1959 Shunryu Suzuki, a Zen Buddhist teacher from Japan arrived in San Francisco and began teaching Zen meditation practices to Americans. The American students that joined Suzuki to sit and study Zen eventually formed the San Francisco Zen Center with Suzuki, one of the first meditation teaching centers in the US. Through the 1960’s -1970’s numerous meditation teachers from Tibetan, Vipassana and Zen Buddhist and Hindu traditions came to Europe and the USA to teach their forms of meditation.
For over thirty-five years there has been a growing movement to both understand the scientific mechanisms of meditation and to de-mystify meditation and make the once esoteric practices available in numerous therapeutic settings. A pioneer in this field is Jon Kabot-Zinn who, in 1979, founded the Mindfulness-Based Stress Reduction (MSBR) Program. at the University of Massachusetts Medical Center, now the Center for Mindfulness at the University of Massachusetts.
This was the first science-based program to use mindfulness mediation to treat patients with chronic illnesses.
From History of MBSR: “MBSR spans a confluence of epistemologies and practices from two very distinct and until recently, divergent lineages, both committed to empirical investigation, albeit utilizing very different methodologies: that of science, medicine, and psychology, on the one hand, and that of Buddhist meditative traditions and their teachings and practices, known collectively as the Dharma, on the other. — Our work over the past thirty-five years has shown consistent, reliable, and reproducible demonstrations of major and clinically relevant reductions in medical diagnoses and in medical patients with a secondary diagnosis of anxiety and/or panic, over the eight weeks of the MBSR intervention, and maintenance of these changes in some cases for up to four years of follow-up.”
Mindfulness and other Buddhist meditation techniques are being advocated in the West by innovative psychologists and expert Buddhist meditation teachers such as S.N. Goenka, Jack Kornfield, Joseph Goldstein, and Sharon Salzberg, who have been widely attributed with playing a significant role in integrating the healing aspects of Buddhist meditation practices with the concept of psychological awareness and healing.
Currently mindfulness and other meditation practices are often taught to elementary school students, prisoners, sports teams, CEOs, caregivers and many other diverse populations. Many medical schools and university neuroscience departments, ie. Brown, UCLA etc, are also studying the connection between meditation and science, the mind/body connection.
So, while health benefis of mediation is a new topic in this blog, this field has a long and venerable history. As you will observe, many of the research citations listed in this blog entry go back to the 1990s and even earlier. Yet, much is still being discovered and the Great Book of Meditation and Science is far from written yet. You will also see very recent publications listed, dealing with new topics such as meditation’s epigenetic impacts and how it affects gene expression. And employing new technology such as functional MRI and new forms of HRV, there is still much to be discovered about how meditation works.
The top 21 Benefits of Meditation- by James P Watson
The benefits are these.
- Meditation reduces stress, ruminative thoughts, appraisals of threat, increases compassion, and may slow the rate of cellular aging
- Meditation reduces heart rate, ambulatory blood pressure and stress-induced hypertension
- Meditation reduces carotid artery intimal thickness (CIMT)
- Meditation lowers lipid peroxide levels in the blood
- Meditation improves Heart Rate Variability (HRV)
- Meditation increases melatonin levels, which helps you sleep. Melatonin also prevents cellular senescence and activates SIRT1 gene expression
- Meditation increases telomerase activity by 43%
- Meditation effectively treats Depression with the same “effect size” as medication
- Meditation reduces mortality
- Meditation down-regulates pro-inflammatory genes – COX2 and RIPK2
- Meditation increases DHEA levels and reverses its age-related decline by 5-10 years
- Meditation increases the size of the brain
- Meditation increases Activity in the Brain’s “Attention Center”
- Meditation Deactivates (decreases activity) in the Brain’s “Daydreaming Center”, also known as the “Default Mode Network”
- Breathing Rate with Meditation Determines the size change of a very specific area under the occipitotemporal lobe. Breathing rate decreases with increasing experience of the meditator
- Meditation can reduce Chronic Pain
- Meditation can reduce anxiety
- Meditation is an “Epigenetic Drug, changing gene expression
- Meditation can reduce stress in caregivers of those taking care of dementia patients and handicapped patents or children
- Meditation changes gene expression in peripheral blood lymphocytes
- Meditation reduces Loneliness in elderly adults
1. Meditation reduces stress, ruminative thoughts, appraisals of threat, increases compassion, and may slow the rate of cellular aging
That sounds like hyperbole from a “blow hard” or recent convert, but it is actually from an article with a Nobel Laureate as a senior author! (Dr. Elizabeth Blackburn). Here is the Reference: 2009 Can Meditation Slow Rate of Cellular Aging? Cognitive Stress, Mindfulness, and Telomeres
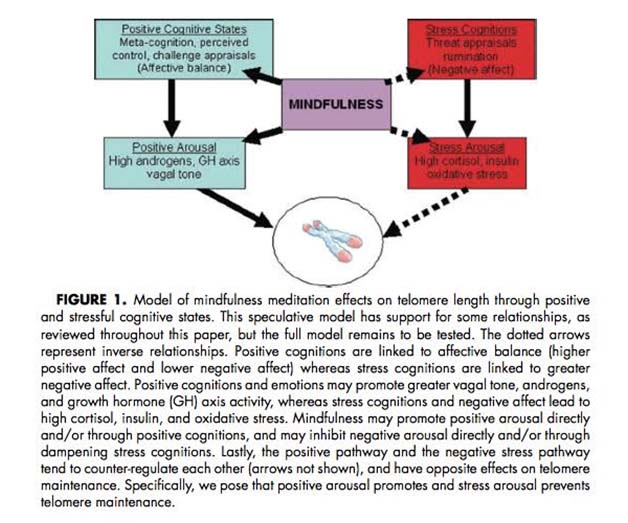
Here is a diagram from that article:
Dr. Blackburn and others have since developed an intense research program on meditation, since it was discovered that meditation can activate the telomerase enzyme better than any drug or supplement. See also the 2010 publication co-authored by Dr. Blackburn Intensive meditation training, immune cell telomerase activity, and psychological mediators.
Several studies including randomized clinical trials have evaluated meditation of various types on reducing stress among normal individuals, among cancer patients, college studies, and among those with essential hypertension. Meditation also increases forgiveness among college students! Who would have guessed? With mindfulness meditation, total Mood Distrubance scores were reduced by 65% with a 31% reduction in the Symptoms of Stress. Another type of meditation is called “compassion meditation”. I like this type. The Dali Lama just celebrated his 80th birthday at the Honda Center here in Los Angeles. Thousands of people and several Nobel Laureates came to celebrate his birthday in this convention center. He gave a talk about the need for “compassion” in the world right now. My friend, Dr. Ray Lam was there and said it was difficult to understand the Dali Lama, but that he was a very moving speaker.
Some studies suggest that mindfulness meditation and relaxation therapy have equal effects on stress. Others have suggest that mindfulness meditation is superior to relaxation therapy, but not all authors agree. Here is a smattering of the relevant articles:
References:
2006 Passage meditation reduces perceived stress in health professionals: A randomized, controlled trial.
-
Meditation reduces heart rate, ambulatory blood pressure and stress-induced hypertension
A randomized controlled clinical trial was done in 2008 by the center for Contemplative Meditation at the U. of Wurzburg, Germany. Normally an article like this would be published in an obscure hypertension journal, but this was published in the Journal of Hypertension AND also in nature.com, Contemplative meditation reduces ambulatory blood pressure and stress-induced hypertension: a randomized pilot trial.
.The Clinical Trial consisted of 52 pharmacologically untreated subjects with essential hypertension. The 52 subjects were randomly allocated to either 8 weeks of contemplative meditation with creating techniques (CMBT) or no intervention. The CMBT consisted of two early morning and evening sessions of training for 40 min in each session. The first 12 minutes of this 40 minute sessions involved teaching the individuals to breathe deeply. The 2nd phase was 30 minutes of meditation based on Christian tradition (that is what they call “contemplative meditation”.) The observers were blinded. The CMBT reduced heart rate (-13% vs 0% in controls) reduced systolic BP (-15 mmHg vs 3mm in controls) and diastolic BP (-13 mmHg vs -2% in controls) and also reduced the scores on the mental stress test (11 mmHg lower BP during mental stress test in the CMBT group).
As it turns out, several prior studies had already shown this effect. These studies are Referenced below:
1995 A randomised controlled trial of stress reduction for hypertension in older African Americans
-
Meditation reduces carotid artery intimal thickness (CIMT)
This was very surprising to me! Carotid artery intimal thickness (CIMT) is supposed to be an irreversible event! In several studies, they showed that it was reduced or reversed.
1996 Stress Management and Health (slide presentation)
2000 Effects of Stress Reduction on Carotid Atherosclerosis in Hypertensive African Americans
1994 George Lyman Duff Memorial Lecture. Arterial imaging and atherosclerosis reversal
-
Meditation lowers lipid peroxide levels in the blood
One study has shown that transcendental meditation reduces lipid peroxide levels in serum. This was another surprise! This study compared long term meditators with controls who did not meditate. This study had 41 patients that were studied, 18 of which were long term meditators and 23 were controls. They showed that the long term meditators had a 15% lower lipid peroxides (measured by TBARS) in their plasma (serum), compared to controls.
Reference: 1998 Lower lipid peroxide levels in practitioners of the Transcendental Meditation program
-
Meditation improves Heart Rate Variability (HRV)
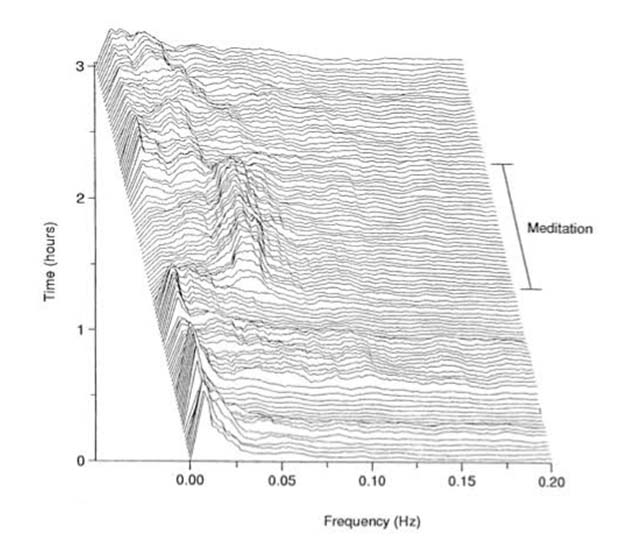
This particular section of this blog is the longest and I am concerned I may lose my audience, so here is the one graph that will convince any scientist or lay person that meditation makes a dramatic change in HRV. This graph is from Harvard Medical School scientists:
Reference: 1999 Exaggerated heart rate oscillations during two meditation techniques
Heart Rate Variability (HRV) is the “beat-to-beat” change in heart rate. It is NOT a measure of heart rate, per se. Whereas a LOW heart rate is generally a sign of health, HIGH heart rate variability is a sign of health. Over 17,895 PubMed research publications have been written on HRV as of this year and the scientific evidence on the importance of this health biomarker is getting stronger and stronger. For instance, in a subset of patients in the Framingham Heart Study that has been ongoing for over 40 years, HRV had an independent predictive value in determining “all cause mortality”. I have written a recent blog on our website about HRV that you may want to read. Digital health – health and fitness wearables, Part 3: Heart Rate Variability: Principles and Science and Practical Measuring Devices.
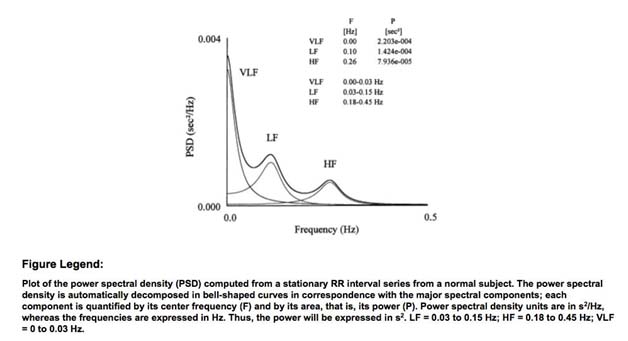
Here is a diagram from the American College of Cardiology on the Frequency Power Spectrum of HRV.
Basically there are two ways of measuring HRV – Time Domain measurements (Ex: R-to-R interval measurements in milliseconds) and Frequency Domain Measurements (see diagram above) which require Fourier transformations (“complicated math”) to derive. Whereas Time Domain measurements are easy to do and quite reproducible, Frequency Domain measurements are much harder to do and typically require sampling of HR over several hours or 24 hours. Thus Holter monitoring data has become the most common method of collecting HRV data in clinical research.
The 10 most important things that change HRV
The following diseases have been shown to depress HRV and the following interventions have been shown to improve HRV:
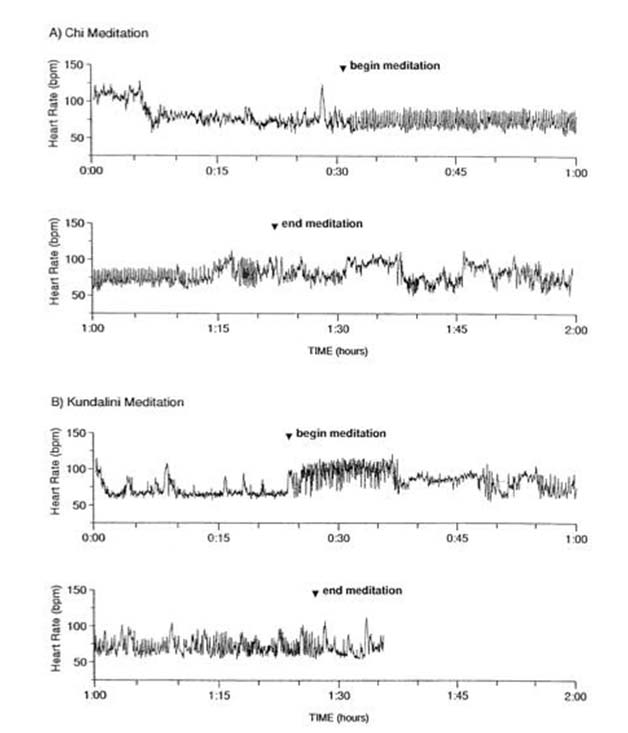
- Meditation – Meditation can have a dramatic positive effect on HRV. There are over 1,000 studies that show this effect. This includes many forms of mediation, including Pranayama meditation, Kundalini Yoga meditation, Chinese Chi meditation, Mindfulness Meditation, and even just deep breathing exercises. The most dramatic changes in HRV that have been found with Chinese Chi meditation and Kundalini Yoga meditation in experience practitioners. In these individuals, dramatic oscillations in HRV occur in the 0.025-0.35 Hz band, which spans the VLF, LF, and HF spectrum. The most dramatic change occurred in the VLF/LF frequency domain below 0.05 Hz. The above 3D illustration of the data (the topographic map) from experienced meditators, shows their HRV power spectrum before meditating, during meditating, and after meditating. A dramatic shift to higher frequencies is shown during meditation.
Not only could this be measured in the power spectrum of HRV, it could also be measured simply with the change in time domain (rMSSD, SDNN, etc.). Experienced practitioners of Chi Meditation and Kundalani Meditation both had fluctuations in the time domain of HRV by as much as 30-35 beats per minute within a 5 second interval! This is a more dramatic increase that even that seen in well-trained endurance athletes! (they compared the meditators with the athletes). Here is a depiction of the same data but in the time domain for Chi Meditation and Kundalani Meditation:
Interestingly, these extremely prominent oscillations in HRV correlated with slow breathing. These HRV oscillations seen during meditation were larger in amplitude than those seen with the respiratory sinus arrhythmia observed during the pre-meditation control state. These HRV oscillations were also much larger than those seen with metronomic breathing (i.e. breathing slowly to a metronome). They were even larger than the HRV oscillations seen at night in elite triathlon athletes during sleep (i.e. nocturnal HRV measurements).
Many other authors have found similar high amplitude, very low frequency/low frequency oscillations in HRV with different types meditation techniques. There does not appear to be one particular meditation technique that has a “monopoly on health”. The HRV oscillations seen with meditation cannot be explained by respiratory sinus arrhythmia (i.e. due to breathing) or changes in autonomic outflow, such as the vagal parasympathetic dominance seen in athletes.
Whereas the old view of mediation was that meditation simply “calmed the heart and mind”, this HRV data contradicts this simplistic view. This data shows that meditation produces an active cardiac dynamic change, not a quiescent cardiac dynamic. This phenomena has been referred to as the “meditation paradox.” The Meditation Paradox is the fact that the HRV evidence does not fit the old “quiescent theory” of what meditation does
Conclusion: Meditation has profound effects on HRV that can be easily measured in both the time domain (R-to-R interval measurements such as rMSSD, SDNN, etc.) and in the frequency domain (VLF, LF, and HF power spectrum). In experienced mediators, large oscillations in HRV occur with changes of 30-35 bpm over 5 seconds in the time domain and large frequency oscillations that spanned 0.0025 to 0.35 Hz range. These findings contradict the conventional wisdom and the “status quo” view of meditation as merely a way of inducing calm or a “homeostatic” state by reducing psychologic stress or lowering breathing rate. In summary, the objective HRV data from meditation shows that it is more than simply “relaxation therapy” or “breathing exercises”. Metronomic breathing does not mimic meditation. .
References:
2003 Heart rate dynamics during three forms of meditation
2008 Changes in heart rate variability during concentration meditation
2002 Effects of Qi-Training on Heart Rate Variability
2009 Effect of integrated yoga on stress and heart rate variability in pregnant women
2006 Effects of two yoga based relaxation techniques on heart rate variability (HRV).
2004 Heart rate dynamics during three forms of meditation
1999 Exaggerated heart rate oscillations during two meditation techniques
In the remainder of this Section on Heart Rate Variability, you will see a number of literature citations pointing to topics discussed commonly in the literature of both meditation and HRV – topics like constitutional stress, impacts of exercise, and nature of sleep. We infer that this is because the mechanisms of action of both sleep and meditation affect the systems and pathways that impact HRV.
- Hypertension, Coronary Heart Failure, and Myocardial Infarction All of these decrease HRV due to reduced parasympathetic activity, which is manifested by a lower “HighFrequency” (HF) in the power spectrum of HRV measurements. In the time domain, HTN, CHF, and MI all decrease the root mean square standard deviation (rMSSD) of heart rate variability measurements. It is not surprising, then to find out that all of the drugs used to treat HTN, CHF, and MI which have been shown to change long term mortality also improve HRV, whereas the drugs that are used to treat HTN, CHF, and MI which did not alter long term mortality did NOT change HRV. Here are some examples:
- Antiotensin converting enzyme (ACE) inhibitors – they lower 5 year mortality and improve HRV
- Digitalis – this does not improve HRV and makes very little difference in 5 year mortality
- Lowered sodium diet – lowering sodium in the diet improves HRV, whereas increasing salt in the diet makes HRV worse. This appears to be mediated by an increase in NO production with a high sodium diet and increased NO sensitivity as an adaptive function due to the high sodium.
References:
2008 Angiotensin II disproportionally attenuates dynamic vagal and sympathetic heart rate controls
2004 Relationships among heart rate variability, hypertension, and relaxation techniques
1996 Role of AT1 receptors in the central control of sympathetic vasomotor function.
- Exercise – Exercise has been shown to dramatically improve HRV. However, during exercise itself, HRV is decreased. HRV does not improve until you have fully recovered from exercise. After exercise recovery, there is an increase in High Frequency (HF) power and lowering of Low Frequency (LF) power. It increases the root mean square of standard deviation in R-to-R intervals (rMSSD). The most important health benefit of exercise may have more to do with improving HRV than they do with any of the other 80 molecular mechanisms that have been scientifically proven to occur with aerobic exercise. Specifically, this may explain some of the benefits of exercise on depression, reducing Alzheimer’s disease, reducing cancer risk, etc.
Since exercise is “free”, exercise is probably the best “drug” to improve your HRV!
References:
2001 Effects of aerobic exercise training on 24 hr profile of heart rate variability in female athletes
1997 Autonomic differences between athletes and nonathletes: spectral analysis approach
2003 Heart rate variability in athletes
2006 [Heart rate variability and physical exercise. Current status].
- Sleep – Sleep has a positive effect on HRV. Although there are differences in HRV between REM and non-REM sleep, a good night’s sleep will make dramatic improvements in HRV during the following daylight waking hours. Interestingly, meditation improves HRV during sleep after cyclic meditation followed by supine rest. This supports the idea that sleep and meditationmay have a synergistic effect on HRV.
References 1969 Reflex Regulation of Arterial Pressure during Sleep in Man
2010 Heart Rate Variability During Sleep Following the Practice of Cyclic Meditation and Supine Rest
- Lack of Sleep and Jet Lag– cutting across time zones and disrupting normal circadian rhythms dramatically decreases HRV. The depressed HRV does not resolve until the “Jet lag” has resolved.
- Stress and Glucocorticoid administration– Stress and steroids both depress HRV. Psychological stress is even worse than glucocorticoids because so many other hormones are also increased with stress, such as epinephrine, norepinephrine, etc.
The mediator of this impaired HRV is hydrogen sulfide signaling.
References:
Glucocorticoids modulate baroreflex control of heart rate in conscious normotensive rats
- Chronic Hypoxia – Chronic hypoxia (such as in sleep apnea or COPD) does not affect heart rate that much but has a dramatic effect on HRV. This is why sleep apnea must be diagnosed and treated in these patients. Likewise, chronic hypoxia induced by rapid elevation gain to high altitude results in a dramatic depression in HRV. However, if one climbs to high altitude slowly and acclimatizes, there may be a transient depression in HRV, but it usually returns to normal unless high altitude illness occurs, such as HAPE or HACE.
References:
2006 Heart rate variability in rats with chronic hypoxic pulmonary hypertension
1996 Effects of high altitude acclimatization on heart rate variability in resting humans.
2008 Effect of rapid ascent to high altitude on autonomic cardiovascular modulation
2005 Autonomic adaptations in andean trained participants to a 4220-m altitude marathon
- Air pollution – Air pollution worsens HRV. A recent study from Harvard’s School of Public Health showed that air pollution in general reduced HRV, but ozone and particulate matter in the air were most associated with a decrease in HRV.
Reference: 2005 Effects of air pollution on heart rate variability: the VA Normative Aging Study
- Happiness vs Depression – Happiness increases HRV whereas depression dramatically reduces HRV. Surprisingly, although antidepressant drugs may reduce symptoms of depression, they do not improve HRV. This suggests that these drugs do not treat the underlying cause of depression, but instead are chemically treating the symptoms of the disease. This is a very sobering thought. On the other hand, meditation improves HRV and effectively treats depression. This suggests that meditation is treating the underlying cause of the disease. One interesting report showed that the effects of negative emotions on HR lasted longer than the effects of positive emotions on HR. This suggests that we “cannot afford” to stay depressed and “wallow in our self pity”
References:
2003 Heart rate response is longer after negative emotions than after positive emotions
2008 Neural correlates of heart rate variability during emotion
- Psychological Stress and Anxiety – Psychological stress worsens HRV. Anxiety also worsens HRV. With normal circadian rhythms, HRV gradually worsens during the day. This may explain why we humans are more vulnerable to the harmful effects of stress when we work long hours or are subject to stressors when we get home from work (i.e. spousal conflicts usually occur in the evening).
References:
2001 Comparison of heart rate variability measures for mental stress detection
-
Meditation increases melatonin levels, which helps you sleep. Melatonin also prevents cellular senescence and activates SIRT1 gene expression
There is strong evidence that meditation increases endogenous melatonin production.
- Although sleep is the obvious benefit of melatonin, there are many other benefits from melatonin because it is a “mitochondrial specific antioxidant.” .
- There is also strong evidence that melatonin has health span and life span enhancing properties through molecular mechanisms that are related to caloric restriction, specifically SIRT1 activation and Nrf2 activation.
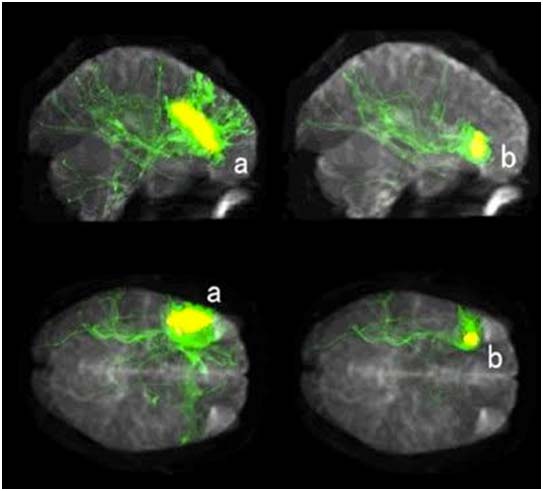
Melatonin may be the most “pleitropic molecule” in the entire body! It has so many effects and so many mechanisms. Functional MRI studies have shown that meditation increases metabolic activity in the pineal gland (see Reference below). Measurements of melatonin levels in long-term practitioners of meditation show statistically significant increases in plasma levels of melatonin in several independent studies (see References below).
There are multiple molecular mechanisms by which melatonin has health-promoting benefits. This includes anti-inflammatory and immune stimulating effects, anti-cancer and chelating properties, anti-oxidant properties. For instance, melatonin has been shown to inhibit NF-kB signaling, thereby reducing inflammatory gene expression. Moreover, melatonin has been shown to increase Nrf2 signaling.
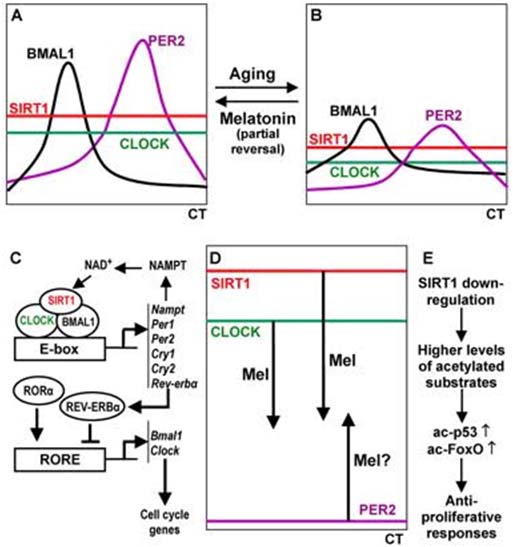
The most fascinating recent molecular mechanism that has been discovered is the effect of melatonin on preventing cellular senescence (see Reference below). More recently, melatonin has been shown to induce gene expression of SIRT1. SIRT1 is one of the major calorie restriction (CR) pathway genes that has been shown to explain part of the molecular mechanisms of CR on health span and lifespan. In 2014, Hardeland published a paper showing evidence that melatonin also exerts its effects through epigenetic mechanisms, noncoding RNAs, and via messenger RNA stability. Here is a simplified illustration on how this works:
Illustration Reference: 2014 Melatonin, Noncoding RNAs, Messenger RNA Stability and Epigenetics—Evidence, Hints, Gaps and Perspectives
Conclusion: Meditation increases melatonin during the day and at night. This effect has widespread effects throughout the entire body due to multiple signaling pathways which are activated by melatonin. This is further evidence that the health and longevity benefits of meditation can no longer be dismissed!
- Meditation increases telomerase activity by 43%
Telomeres are the “caps on our chromosomes” that protect our chromosomes from forming bridges (translocations) with other chromosomes. With aging, our telomeres shorten due to the “end replication problem”, which is the shortening of the end of the DNA strand when it is copied by DNA polymerase with cell division. However, if cell division was the only cause of telomere shortening, then everyone’s telomeres would shorten at the same rate. In real life, this is not the case. What basic science researchers have discovered is that cellular stress accelerates telomere shortening. When the telomere gets too short, it triggers the “DNA damage response” which then causes the cell to die or to undergo cellular senescence. Fortunately, there is an enzyme that lengthens the telomeres called “telomerase”. Telomerease was discovered by Dr. Elizabeth Blackburn (at UCSF) and two other researchers. They won the Nobel Prize in 2008 for their discovery over 30 years ago.
Reference: 2010 Intensive meditation training, immune cell telomerase activity, and psychological mediators. “RESULTS: Telomerase activity was significantly greater in retreat participants than in controls at the end of the retreat (p<0.05). Increases in Perceived Control, decreases in Neuroticism, and increases in both Mindfulness and Purpose in Life were greater in the retreat group (p<0.01). Mediation analyses indicated that the effect of the retreat on telomerase was mediated by increased Perceived Control and decreased Neuroticism. In turn, changes in Perceived Control and Neuroticism were both partially mediated by increased Mindfulness and Purpose in Life. Additionally, increases in Purpose in Life directly mediated the telomerase group difference, whereas increases in Mindfulness did not. — CONCLUSIONS: This is the first study to link meditation and positive psychological change with telomerase activity. Although we did not measure baseline telomerase activity, the data suggest that increases in perceived control and decreases in negative affectivity contributed to an increase in telomerase activity, with implications for telomere length and immune cell longevity. Further, Purpose in Life is influenced by meditative practice and directly affects both perceived control and negative emotionality, affecting telomerase activity directly as well as indirectly.”
Interestingly, “Relaxation therapy” does not turn on the telomerase enzyme, but meditation does activate telomerease by 43%. This was a surprising study that was published in 2012. This was after an 8 week training course in meditation. (Without the meditation course, the control group who did not meditate had no increase in telomerease activity).
Three other studies have been done since then that have confirmed this finding. A meta-analysis of these 4 studies has been already done and concluded that the data was strong enough to believe. They suggested a long term trial to verify that telomere length increases would result from this increase in telomerase enzyme activity. However, so far no long term studies has been done to prove that the “meditator” telomeres increase in length. What we do know is that telomerase activity clearly increases more dramatically with meditation than any telomerase supplement that has ever been devised or sold.
Conclusion: Mindful meditation and other forms of meditation clearly increase telomerase activity. Whether this is due to an increase in gene expression or a decrease in telomerase enzyme inhibition by other factors such as the long noncoding RNA, TERRA, is still not yet known. Whether meditation will actually increase telomere length is also not yet known, but this is the most effective thing that has ever been found to increase the telomerase enzyme activity.
- Meditation effectively treats Depression with the same “effect size” as medication
There is very strong scientific evidence that meditation has profound benefits for treating depression. The first Reference below is a doctoral dissertation on the effects of meditation on depression. Randomized controlled trials of mindfulness meditation training have also been done which show objective measurements of improvement in sleep and mood. Both Major Depressive Disorder (MDD) and Unipolar depressive syndromes and recurrent brief depressive disorder have been shown to improve with meditation. A recent study out of Johns Hopkins by Dr. Madhave Goyal, MD, MPH, reviewed 18,000 earlier studies on depression and ultimately arrived at 47 quality studies that had been done as randomized clinical trials (RCTs) to study the effects of meditation on depression. Together, the number of patients in these 47 RCTs was over 3,500 patients. All of these patients were either randomized to meditation (mindfulness or mantra) or another treatment like exercise. The results of this meta-analysis showed that the “effect size” for meditation on depression was 0.3.
In other studies that looked at medications for depression, a similar “effect size” of 0.3 has been found. The best results of treating depression with meditation involve an 8-week training period. The studies showed that as little as 2.5 hours of meditation per week is adequate to show a benefit for depression. Most of these programs are called “Mindfulness-Based Stress Reduction”.
References:
2014 For Depression Treatment, Meditation Might Rival Medication
2006 MEDITATION AND DEPRESSION
2014 Mindfulness Meditation Can Help Relieve Anxiety And Depression
- Meditation reduces mortality
Mortality in the Elderly w/ and w/o Mediation
A randomized, prospective study of TM was done by Alexander and colleagues from Maharishi International University in Fairfiled, Iowa in 1989. Reference: 1989 Transcendental meditation, mindfulness, and longevity: an experimental study with the elderly
In this study, they looked at mortality in a group of elderly volunteers in rest homes with an average age of 81.After one year, the transcendental group showed a significant improvement in quality of life and BP. After 3 years, the number of surviving in the meditation group was significantly higher than in the non-meditating group. Even in the 15-year follow-up study, there was a lower cardiovascular mortality rate than in the control group.
At the 2015 Paul Glenn Conference on Aging at Harvard, Vince heard Dr. Elisbeth Blackburn talk about depression and telomere length being very accurate predictors of mortality. If we understood correctly, 100,000 individuals were tracked over a 5 year period by the researchers. They looked at dozens of biomarkers for health and longevity. The study was sponsored by Kaiser Permanente and was conducted by several Kaiser physicians as well as Dr. Elizabeth Blackburn from UCSF. In this study, they found that patients with major depression had a higher rate of “all cause mortality”, but depression alone could not reliably predict 5-year mortality rates. Likewise, shortened telomeres also predict mortality, but telomere length alone did not reliably predict 5-year mortality. However, when both depression and short telomere data was combined, the two biomarkers predicted a 100% mortality over the subsequent 5 years. This is the most indicative 5-year biomarker of mortality we have encountered that does not involve a deadly disease process.
Conclusion: This study has not yet been published, but when it does, all doubts about the importance of mental health and telomeres will be dispelled. No other biomarkers can predict 5-year mortality as accurately as major depression and telomere length, except a few for absolutely deadly diseases like glioblastoma. Meditation may be the only intervention that both directly affects depression and telomere length.
-
Meditation down-regulates pro-inflammatory genes – COX2 and RIPK2
This was a real surprise. Researchers found that RIPK2 and COX2 were down regulated in PBMCs with meditation. Meditation also reduced C-reactive protein gene expression in another study.
References:
2014 Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators
-
Meditation increases DHEA levels and reverses its age-related decline by 5-10 years
DHEA-S levels in meditators was higher in all 11 age groups studied, in both male and female, and was independent of diet, BMI, and exercise.
Dehydroepiandrosterone sulfate (DHEA-S) is a “pre-hormone” that can be used by your body to make testosterone (in the testes) and estrogen/progesterone (in the ovaries). More importantly, testosterone, estrogen, and progesterone are all neurohormones that are needed in the brain for normal neurogenesis in males and females. Unfortunately both DHEA-S levels decline with aging and so does the production of sex-steroid neurohormones in the brain.
In several studies, DHEA-S levels in serum (blood) was measured and found to be higher in meditators vs non-meditators. This finding was consistent in all 11 age categories studied and amounted to a 5-10 year “younger DHEA-S level”. More importantly, this effect was independent of body mass, exercise, and diet. In trials of oral DHEA-S administration, researchers have documented increases in more than just sex steroid hormones. For instance, in one trial of 100mg/day of DHEA-S, serum androsternedione, testosterone, and dihydrotestosterone all increased to levels above gender-specific ranges in women, but not in men (in men, the effect was not as dramatic). DHEA administration also increased serum IGF-1 levels by 16% in men and 31% in women. Body fat decreased in males (1 kg or 6% of body weight) but not in females. In men, knee muscle strength lumbar back strength both increased. All of these changes were statistically significant in this study that was carried out for 6 months.
Conclusion: Meditation induces the endogenous synthesis of DHEA-S. I think this is remarkable. Although the exact molecular mechanism of how meditation induces DHEA-S synthesis is still unknown, what is clear is this – endogenous DHEA-S synthesis is always better than exogenous dietary intake. With increased endogenous synthesis of any hormone, that synthesis is net of any “feedback inhibition effect” on endogenous production of the hormone. With exogenous administration, there always can be a “feedback inhibition effect” which results in decreased endogenous production of a hormone. For this reason, meditation may be a “superior way to get your DHEA“.
References:
-
Meditation increases the size of the brain
Grey matter and white matter both increase in specific areas, including right orbitofrontal cortex, middle frontal cortex, superior frontal cortex, right insula, funds of the central sulcus, right middle and frontal sulci, left superior temporal gyrus, and left inferior temporal gyrus.
Summary: Specific areas of the brain increase with meditation. Both white matter and grey matter volume change with regular meditation and prevent the age-related decline in brain volume!
This was one of the most shocking thing I have ever read. The evidence is recent.- just in the past 10 years since 3D MRI and Diffusion Tensor Imaging (DTI) have been developed. The research has been done at MIT, Massachusetts General Hospital, Harvard University, Duke University, Florida State University, UCLA, and many other institutions. There is not one “select type of Mediation” that is better at this than the rest. Meditation techniques from Buddhist meditation (Zazen, Samantha, and Vipassana) and Hindu yoga/meditation techniques such as asanas yoga (position) and pranayama yoga (breathing meditation) all seem to work. Meditation changes cortical volume (grey matter) and subcortical volume (white matter) in individuals who meditated on a regular basis – affecting only specific regions of the brain. Most participants in the MRI studies had meditated for an average of 8-9 years for 40 minutes/day to as much as 2 hours per day.
This evidence is objective and cannot be debated or dismissed! It was statistically significant with p = 0.00001 in some cases! This is the strongest kind of scientific evidence – you cannot alter this like you can with answers on a questionnaire! The enlargement of the brain was not diffuse – it was very specific in location. It was also specific to the side of the brain. Here are the locations where the brain gets bigger (note where it enlarged preferentially on one side)
– Right OFC – the grey matter of the right Orbitofrontal cortex (OFC) which is involved with emotional control gets larger! This region seemed to be the most consistently enlarged in all of the studies, although there were some exceptions. This was measured with MRI, functional MRI, SPECT scans, and PET scans.
– MFC & SFC – the grey matter of the middle and superior frontal cortex (MFC and SFC) enlarged –
– Right Insula – The grey matter in a large area of the right insula enlarged – this is Broadman’s area 9. It is activated by tasks of interoceptive awareness. The observations of bodily sensations during meditation may be why this area enlarged in meditators
– Fundus of central sulcus – The grey matter in the fundus of the central sulcus was also enlarged – this is Broadman’s area 3a
– Right Middle and Frontal sulci – The grey matter the right middle and frontal sulci enlarged – this is Broadman’s area 10. p = 0.002
– Left Superior temporal gyrus – The grey matter in the left superior temporal gyrus enlarged – this is the auditory cortex
– Left inferior temporal gyrus – This area not only enlarged, but the enlargement correlated with the number of years that the meditator had been doing meditation. The left temporal lobe has been connected with spiritual activity and mysticism in many EEG studies and functional MRIs. This is the region where “deep pleasure” is felt and the experience of insight into the “unity of all reality.”
– Right Hippocampal gyrus – The hippocampus enlarged in one study – obviously this would be great for short term memory (see Reference below). The reason why they thought that the hippocampus enlarged with meditation was due to its role in modulating amydalar activity and thus its role in attention and emotional activity
– Putamen – one study found that the area with the greatest change in grey matter volume was the putamen. The putamen is very important in processing attention and may help with attention deficit disorders (ADHD)
What was even more notable was that in control brains (those that did not meditate), the brains underwent normal, age-related decline in volume! (p = 0.001). This should be enough evidence for everyone that meditation works.
Here are the References:
2012 The effect of meditation on brain structure: cortical thickness mapping and diffusion tensor imaging
2006 Meditation experience is associated with increased cortical thickness
2007 Age effects on gray matter volume and attentional performance in Zenmeditation
2008 Investigation of mindfulness meditation practitioners with voxel-based morphometry
2012 The Unique Brain Anatomy of Meditation Practitioners: Alterations in Cortical Gyrification
2008 “Thinking about Not-Thinking”: Neural Correlates of Conceptual Processing during Zen Meditation
-
Meditation increases Activity in the Brain’s “Attention Center“
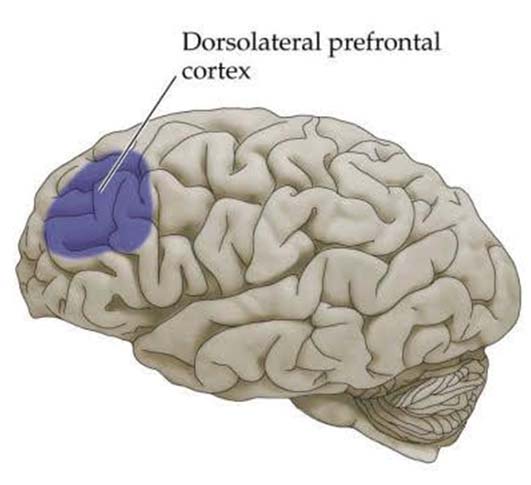
Increased brain activity is seen in the areas of the brain involving attention regulation with meditation – the dorsolateral prefrontal cortex (DLPFC) and the anterior cingulate cortex (ACC).
Recently, functional MRIs (fMRI) have been developed that can actually measure brain activity during meditation. These studies have shown that metabolic activity in the two regions involving attentiveness is increased with meditation. These two areas are located on the outside of the front of the brain (called the “Dorsolateral prefrontal cortex” (DLPFC)and the “anterior cingulate cortex” (ACC). These two regions are involved with attention during the day, and with organizing thoughts. At night, the DLPFC is busy with dreaming, specifically “lucid dreams”, which are associated with REM sleep. Expert meditators with many hours of meditation experience (> 19,000 hours) had more activation of these areas invoking attention. These regions of the brain are located in the illustrations and the picture below:
Illustration Reference: 2012 The Dorso-lateral Prefrontal-Cortex and Lucid Dreaming
Illustration Reference: 2014 How meditation helps with “emotional sobriety”!
Photo Reference: 2008 Extract from The Secret Life of the Brain
References:
2010 Regional Brain Activation during Meditation Shows Time and Practice Effects: An Exploratory FMRI Study
2007 Neural correlates of attentional expertise in long-term meditation practitioners
2000 Functional brain mapping of the relaxation response and meditation
-
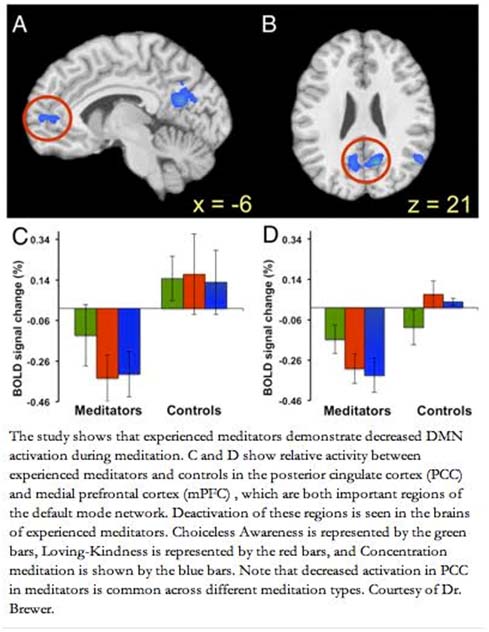
Meditation Deactivates (decreases activity) in the Brain’s “Daydreaming Center”, also known as the “Default Mode Network”
In the posterior cingulate cortex and the medial prefrontal cortex areas, meditation decreased the activity of the brain, reducing mind wandering and daydreaming. This occurred during mediation and after meditation.
Researchers at Yale have recently shown with the same functional MRI technique that there are areas in the brain that account for mind wandering and daydreaming. These activities are not helpful to getting things done and are a great distractor from concentrating on the “task at hand”. At Harvard, some other researchers showed that subjects daydreamed during nearly 50% of their waking hours. This made them unhappy and led them to create the catch phrase, “A Wandering Mind is an Unhappy Mind”. To date, meditation is the only thing that has really been shown to reduce mind wandering. Here are some pictures of how much the activity is decreased with meditation in these two regions:
– posterior Cingulate Cortex (PCC) –
– medial prefrontal cortex (mPFC)
llustration Reference: 2012 The Healing Art of Meditation
References:
2006 Dissociating medial frontal and posterior cingulate activity during self-reflection
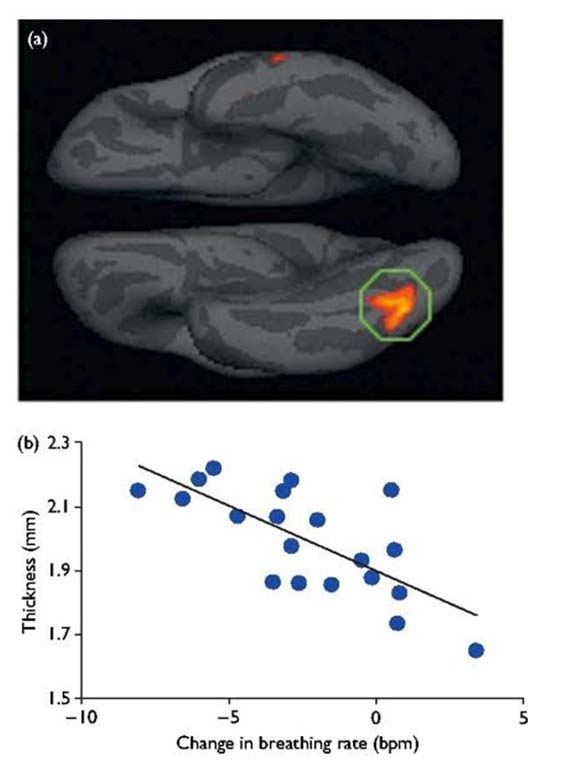
- Breathing rate with meditation determines the size change of a very specific area under the occipitotemporal lobe. Breathing rate decreases with increasing experience of the meditator
– the inferior occipito-temporal visual cortex changes in size based in the meditation breathing rate.
– The meditation breathing rate is a function of how many years a person has been meditating. This relationship is measurable and objective!
All this scientific, objective evidence has been recent – the past 10 years. What several studies have shown is that if you measure the breathing rate of the subject (meditator) before he/she starts meditating, then measure the person’sr breathing rate in the middle of meditating, then subtract the two, you come up with a “∆ RR”, or the change in respiratory rate with meditation. What the researchers found out was that the experienced meditators had greater “∆ RR” than the inexperienced meditators. Once this was discovered, this was used as a “gauge” of mediation experience and to rule out people who were not really meditating.
Instead of just questioning a long term meditator about their meditation frequency, studies have shown that the breathing rate of meditators during meditation is a more sensitive predictor of actually how long meditators have actually been meditating (in other words, many people say they meditate regularly, but really don’t do so). In long-term meditators who actually do the meditation, their breathing rate is lower during the time they are meditating. This is NOT “fakable”. For this reason, Harvard and MIT researchers used the breathing rate of long term meditators to make the following graph and brain image:
Here is what they found – the left inferior occipitotemporal lobe region increased in size and correlated with the “∆ RR
Picture/graph Reference: 2005 Meditation experience is associated with increased cortical thickness
Conclusion: The scientific evidence is clear – the longer you have been meditating (in years), the greater the change in breathing rate occurs with meditation. The greater the breathing rate changes, the thicker the brain cortex gets in the left inferior occipitotemporal lobe region of the brain. Thus it appears that the change in the thickness of the left inferior occipitotemporal lobe region is a direct measurement of breathing rate during meditation.
-
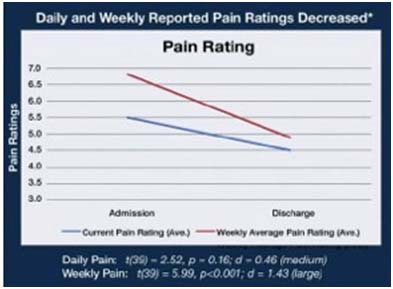
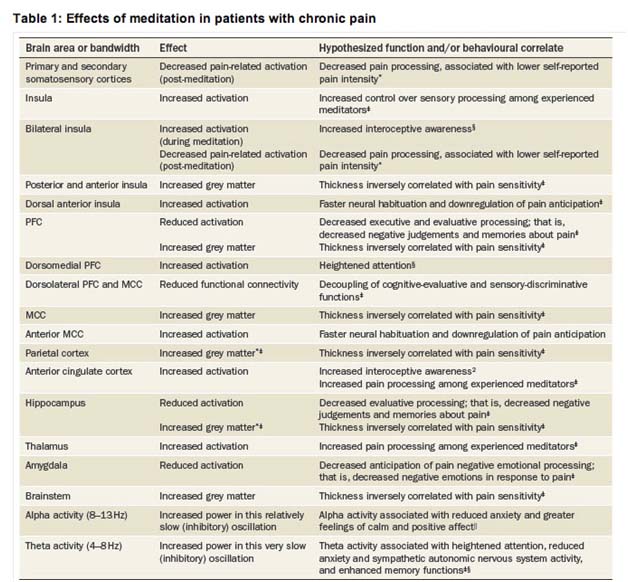
Meditation can reduce Chronic Pain
4 days of meditation decreased pain unpleasantness by 57% and pain intensity ratings by 40%. This effect is probably mediated by increased activity in the anterior cingulate cortex (ACC), anterior insula, and a decreased activity in the thalmus and activation of the orbitofrontal cortex. This was accomplished without drugs and the benefits extended past the period of meditation.
Researchers at Wake Forest University showed that meditation can also reduce pain. They had subjects with chronic pain voluntarily enroll for a multi day course on mindfulness meditation. After only 4 days of meditation, their pain had dramatically reduced in intensity. This included a 57% drop in pain unpleasantness and a 40% drop in pain intensity. This was calculated to be not due to chance. Functional MRIs showed changes in brain activity as explained above
– increase in activity in the anterior cingulate cortex
– increase in activity in the anterior insula
– decreased activity in the thalamus
– increased activity in the orbitofrontal cortex
Other studies have shown reductions in chronic pain with 10 weeks of mindful meditation. At 10 weeks, 65% of patients showed a reduction of > 33% of mean total rating of pain and 50% of participants showed a reduction of > 50% in mean total rating of pain. Another study showed that meditation can reduce low back pain. This was a randomized study. Another study showed that brief mindfulness meditation training reduced experimental pain and that the echanism of action was via the reduction in anxiety (this may be why Valium reduces pain)
One of the most interesting studies was done in a Yoga master who claimed to not feel pain while meditating. In this Yoga Master, MEG and functional MRI studies showed the following:
– on Magnetoencephalography (MEG), pain-related cortical activity on the primary and secondary somatosensory cortices were weak or absent
– on functional MRI, there was a reduced activity during meditation in the thalamus, the insula, and the cingulate cortex
Meditation has even been shown to reduce pain in fibromyalgia in 51% of patients treated with meditation. Thus, meditation is a scientifically validated method for the self regulation of chronic pain and the specific regions of the brain that meditation regulates chronic pain is well established.
Here is a graph showing the pain rating scale before and after meditation:
Reference: Chronic Pain And The Role Of Mindfulness Meditation
Here is a summary of the effects of meditation on pain, from the scientific journal, Nature
Table reference: 2014 Neuromodulatory treatments for chronic pain: efficacy and mechanisms
Here is a table comparing four non-drug methods for controlling pain:
- Hypnosis
- Meditation
- Transcrainial magnetic stimulation
- Neurofeedback
| Treatment | Advantages | Disadvantages |
| Hypnosis | Moderate evidence supports short-term and long-term efficacy Encourages self-management and self-efficacy Few (if any) negative side effects Numerous beneficial side effects (for example, increased global well-being) Evidence supports effects on most neurophysiological processes involved in pain processing—supports potential benefits for a wide variety of pain problems |
Outcome is variable: not everyone benefits Treatment requires patient involvement and motivation |
| Meditation | Preliminary evidence is promising Encourages self-management and self-efficacy Few (if any) negative side effects Reported beneficial side effects include increased well-being Preliminary evidence supports effects on brain structures involved in attention, emotional processing and pain |
Evidence for efficacy not yet well-established Treatment requires patient involvement and motivation fMRI and EEG studies examining the neural correlates of meditation training among novices with chronic pain is lacking |
| Noninvasive brain stimulation (repetitive transcranial magnetic stimulation and transcranial direct current stimulation) | Preliminary evidence for short-term effects is promising Treatment requires minimal patient effort |
Requires equipment Must be provided in the clinic (home practice not yet possible) Passive treatment (does not encourage self-efficacy) Evidence for long-term benefits is lacking; preliminary evidence suggests that benefits may be temporary Associated with minor transitory side effects (for example, fatigue, scalp irritation, dizziness) Mechanisms not yet understood |
| Neurofeedback (EEG and real-time functional MRI biofeedback) | Preliminary evidence for short-term benefits is promising Encourages self-management and self-efficacy |
Requires equipment Effects appear to be weak Evidence for long-term benefits is lacking Mechanisms not yet understood Treatment requires patient involvement and motivation |
Table reference: 2914 Table 2: Neuromodulatory chronic pain treatments: advantages and disadvantages
Summary: The effects of meditation in reducing pain is undeniable and scientifically irrefutable. It works!
References:
2011 Brain Mechanisms Supporting the Modulation of Pain by Mindfulness Meditation
1985 The clinical use of mindfulness meditation for the self-regulation of chronic pain
2010 The Effects of Brief Mindfulness Meditation Training on Experimentally Induced Pain
Beautiful Work: a Meditation on Pain (book extract)
2013 Loving-Kindness Meditation for Chronic Low Back Pain – Results From a Pilot Trial
2005 Intracerebral pain processing in a Yoga Master who claims not to feel pain during meditation
1993 The impact of a meditation-based stress reduction program on fibromyalgia
-
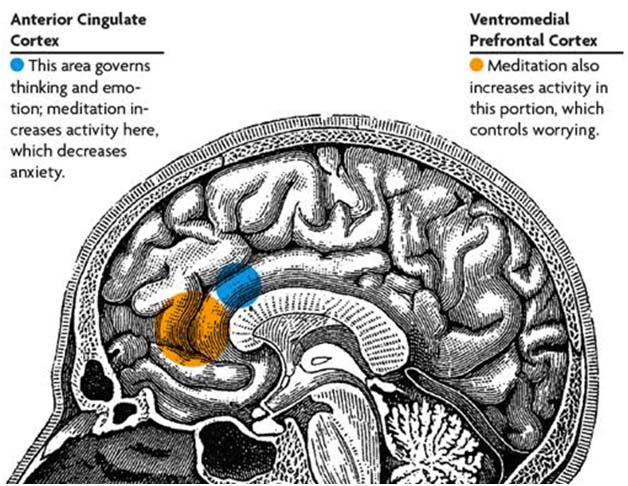
Meditation can reduce anxiety
There is very strong evidence-based medicine that meditation reduces anxiety by activating the anterior cingulate cortex, activating the ventromedial prefrontal cortex, and activating the anterior insula. Transcendental meditation is more effective than placebos, relaxation response therapy, EMG-biofeedback, mantra meditation, PMR, and other relaxation methods. Meta-analysis of the data is robust. Meditation reduces anxiety as effectively as exercise and can be done with “spirituality” or without “spirituality.”
Drugs are not the only way to treat anxiety. Several studies have shown that meditation can make dramatic improvements on reducing anxiety. Meditation can be taught and practiced with a “spiritual side” or without a “spiritual side” There is, however, some evidence that including the spiritual aspect of meditation makes meditation more effective in treating anxiety (see References).
Unfortunately, patients with high anxiety have a low frequency of compliance with mediating (i.e. they don’t do it). This makes the efficacy of treating anxiety with meditation questionable
Another old study showed that aerobic exercise (70% of maximal activity) and meditation had an equal effect on reducing anxiety. A recent randomized controlled trial of meditation for the treatment of anxiety showed a reduction in anxiety, a reduction in blood pressure, but no change in a self-reported depression rating scale. On functional MRI, the following regions of the brain were affected:
– activation of the anterior cingulate cortex (ACC)
– activation of the ventromedial prefrontal cortex (vmPFC)
– activation of the anterior insole
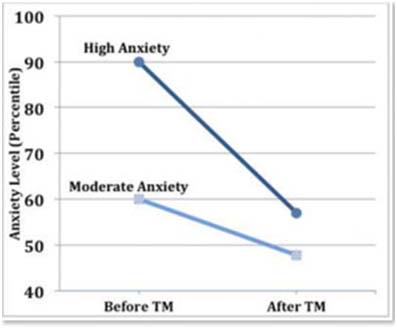
Here is a graph of the effects of meditation on high anxiety and moderate anxiety from a recent meta-analysis:
Graph reference: Trait anxiety and Transcendental Meditation meta analysis
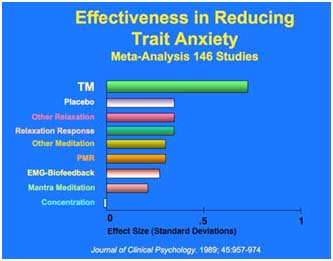
Here is a graph comparing the different types of meditation and stress reduction on treating anxiety (i.e. comparing efficacy)
Graph reference: Why Meditate – The Benefits of Transcendental Meditation
Conclusion: There is more literature on the effectiveness of meditation on reducing anxiety than any other category. This positive benefit of meditation on anxiety stood up in a meta-analysis of the data. Below are just a few of the many References on this topic.
The evidence is very strong – it works!
References:
1993 The impact of a meditation-based stress reduction program on fibromyalgia
2007 Does mindfulness meditation improve anxiety and mood symptoms? A review of the controlled research
1985 Meditation and anxiety reduction: A literature review
1979 Effects of Zen meditation on anxiety reduction and perceptual functioning
2013 Neural correlates of mindfulness meditation-related anxiety relief
2003 Alterations in Brain and Immune Function Produced by Mindfulness Meditation
1978 Anxiety reduction following exercise and meditation
1978 Anxiety reduction following exercise and meditation
2010 The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review
2014 Mindfulness Meditation Can Help Relieve Anxiety And Depression
-
Meditation is an “Epigenetic Drug, changing gene expression
Meditation changes gene expression of histone deacetylase genes (HDAC2, HDAC3, and HDAC9) in peripheral blood lymphocytes in meditators. This alters global histone modification marks like H4 acetylation and H3K4 trimethylation.
Reference: 2014 Rapid changes in histone deacetylases and inflammatory gene expression in expert meditators
-
Meditation can reduce stress in caregivers of those taking care of dementia patients and handicapped patents or children
The type of meditation used was Kirtan Kriya Meditation (KKM) vs listening to music for 12 minutes daily for 8 weeks. The KKM reversed the dysregulation of NF-kB and IRF genes, whereas the music listening did not.
References:
2004 A Pilot Study of a Yoga and Meditation Intervention for Dementia Caregiver Stress
-
Meditation changes gene expression in peripheral blood lymphocytes
This has now been reported by several groups and is statistically significant.
Reference: 2013 Regulation of gene expression by yoga, meditation and related practices: A review of recent studies
- Meditation reduces Loneliness in elderly adults
This was a prospective, randomized controlled trial done at UCLA. The list of genes was quite large and the change in expression was quite mild, however.
References:
2011 Intensive meditation training, immune cell telomerase activity, and psychological mediators
2009 Can meditation slow rate of cellular aging? Cognitive stress, mindfulness, and telomeres
2013 Loving-Kindness Meditation practice associated with longer telomeres in women
2014 A meta-analytic review of the effects of mindfulness meditation on telomerase activity
2005 Studies of chinese original quiet sitting by using functional magnetic resonance imaging
2000 Acute increases in night-time plasma melatonin levels following a period of meditation
1995 Meditation, melatonin and breast/prostate cancer: hypothesis and preliminary data
2008 Evaluation of potential pro-survival pathways regulated by melatonin in a murine senescence model
2008 The SIRT1 Deacetylase Suppresses Intestinal Tumorigenesis and Colon Cancer Growth
2007 Forced and Non-forced Chinese Meditation Studies
2000 Acute increases in night-time plasma melatonin levels following a period of meditation
2004 The effects of long meditation on plasma melatonin and blood serotonin
Final comments – by Vince Giuliano
How does meditation work?
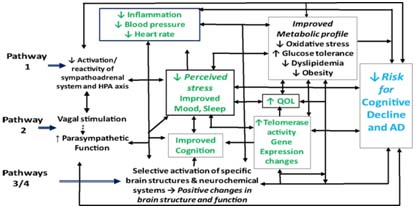
What molecular mechanisms are at work to produce the impressive list of beneficial impacts outlined above? We will probably generate another blog entry on that topic soon, or possibly a series of blog entries. As a teaser consider this image:
Image source: Meditation as a therapeutic intervention for adults at risk for Alzheimer’s disease – potential benefits and underlying mechanisms: Figure 1. Possible pathways by which meditation may improve health outcomes in adults with cognitive impairment
We see in the diagram a number of themes touched on in this blog entry, including the impacts of meditation on reducing inflammation, reducing perceived stress, improving metabolic parameters, upgrading telomerase activity and reducing risk of cognitive decline.
Moreover, the aforementioned article emphasizes the importance of minimizing constitutional stress. “Chronic stress can contribute to a vicious cycle that may not only have deleterious effects on health and cognitive function (32), but ultimately increase risk for institutionalization (29, 30).
The chronic stress that often characterizes the lives of those with cognitive impairment, as well as their caregivers, has been linked to adverse changes in sleep (30), mood (33, 34), and immunological function (33, 35), and elevated risk for metabolic syndrome, cardiovascular disease (CVD), and mortality (36, 37). Chronic psychological stress can have profound effects on memory and behavior in persons both with and without cognitive impairment, and has been prospectively linked to increased risk for incident MCI and dementia in older adults, and to accelerated cognitive decline (38–40). Chronic stress leads to deleterious neuroendocrine and associated inflammatory changes, to suppression of IGF-1 and other neuroprotective factors, and to impaired synaptic plasticity, suppressed neurogenesis, reduced neuronal survival, and other adverse morphological and functional changes in the hippocampus, prefrontal cortex, and other brain structures; all these changes can profoundly affect mood, sleep, memory, and learning (41–45). A large body of experimental, clinical, and epidemiological research has also implicated chronic stress and associated sympathoadrenal activation in the etiology of hypertension, obesity, dyslipidemia, and other components of the metabolic syndrome, and in the development and progression of CVD, type 2 diabetes, depression, and related chronic disorders (41, 46). These disorders have, in turn, been shown to predict cognitive dysfunction, and to increase risk for the development and progression of AD (47–54). Autonomic and hypothalamic pituitary adrenal (HPA) axis dysfunction has also been linked directly to cognitive decline, and to adverse changes in brain structure and function. For example, HPA axis activation, manifested by elevated cortisol levels, has been associated with hippocampal volume loss and memory impairment in non-demented elders (41, 55). As noted above, depression and other mood disorders are common in those with and at risk for AD, including adults with MCI and SCI (12, 13, 28, 56). Depressive symptoms and other distressful states have also been linked to significantly increased risk for diabetes, CVD, stroke, and the metabolic syndrome (57–59), and are a significant contributor to the profound reductions in quality of life reported by those with cognitive impairment (12, 31). Anxiety and depressive symptoms are also significant predictors of cognitive decline and incident cognitive impairment (60, 61). Moreover, in those with MCI, behavioral and psychological symptoms, including anxiety, depression, irritability, and apathy, are strong predictors of progression to AD (28, 62). In addition, mood disturbance can contribute not only to impairment of memory, but also to sleep disturbance, HPA axis dysregulation, and autonomic dysfunction and related pro-inflammatory changes, thus helping to promote a vicious cycle of adverse physiologic, neuroendocrine, and psychosocial changes that foster the development and progression of AD, CVD, and related chronic conditions (41, 63, 64).”
From the 2009 publication Can meditation slow rate of cellular aging? Cognitive stress, mindfulness, and telomeres: Meditation and Stress arousal: “In addition to mitigating stress-related cognitions and emotions, some types of meditation appear to reduce markers of stress arousal, both through the HPA axis, increasing vagal tone, and reducing markers of sympathetic arousal. Transcendental meditation (TM), a concentrative technique that uses silent repetition of a word or phrase as the object of awareness, has been the most extensively studied meditative technique. It appears to reduce systolic and diastolic blood pressure to levels comparable to pharmacologic treatment 116 and improves heart rate variability compared to an active control group.117 It also appears to lower basal cortisol and lead to greater cortisol peaks in response to an acute stressor,118–120 a profile that might be described as enhanced allostasis.38, 121 TM and a similar type of concentrative meditation (the relaxation response technique) are also characterized by decreased oxygen consumption,122, 123 carbon dioxide elimination,124, 125 and salutary EEG patterns (theta and alpha activation).126 — Little research has evaluated specifically the effects of mindfulness meditation on HPA axis arousal or autonomic activity127 although similar effects as those found with transcendental meditation and the relaxation response could be predicted to occur. In one uncontrolled MBSR intervention study, cancer patients consistently showed decreased daily average cortisol values after one year of follow-up .128In a second study, lower cortisol responses to mental stress were observed after five days of practicing an integrated mind-body meditation approach incorporating mindfulness compared to a randomized relaxation control group.129 However, one caveat is that mindfulness includes acknowledgement of distressing thoughts and feelings, which may initially increase arousal and emotional activity, but viewed as a developmental process, may progressively lead to decreased reactivity through enhanced awareness, tolerance of discomfort, and acceptance. Thus, for beginners, and periodically for experienced practitioners, mindfulness meditation is expected to produce increases in physiologic arousal.130.
— Several randomized controlled trials have demonstrated the effectiveness of CBSM (Cognitive Behavioral Stress Management) on reducing peripheral stress arousal. CBSM training reduced urinary free cortisol and epinephrine in clinical samples.131, 132 In one study of healthy participants, CBSM led to lower cortisol reactivity in response to a standardized laboratory stressor within 2 weeks104 and, to a lesser extent, four months after the intervention.133 To the extent that mindfulness or other forms of meditation promote the ability to buffer oneself from social evaluative threat — recognizing that negative social judgments or reflected appraisals of the self (what one thinks others think about oneself) do not necessarily represent reality or a threat to one’s self-worth, practitioners should indeed become less stress reactive.
— Although concentrative and mindfulness meditation techniques may reduce HPA axis and autonomic arousal, the brain appears to respond to specific types of meditation in ways that may represent an adaptive attentional state to appraise stimuli. An fMRI study of meditation practitioners (who practiced Kundalini meditation in which focused attention on respiration is linked to silent repetition of a phrase found increased activation of localized neural structures involved in attention (frontal and parietal cortex) and control of the autonomic nervous system (pregenual anterior cingulate, amygdala, midbrain, and hypothalamus) compared to a control nonmeditative condition.134These data suggest that as some meditation practices produce deep physical relaxation evidenced by reductions in autonomic and HPA arousal, these practitioners were engaged in an active attentional state of autonomic control, countering the notion that meditation is a state of mental as well as physical relaxation. –
Further evidence suggests that meditation effects are not simply the result of volitionally reduced peripheral arousal. Results of a study comparing neural correlates of mindfulness meditation and respiratory biofeedback found that while some regions are engaged by both tasks, mindfulness meditation activates additional neural regions (e.g., right anterior insula).135 Thus, while some forms of meditation engage attentional resources to induce a hypometablic state beneficial for managing stress-related arousal, they also appear to modulate cognitive and emotional processes involved in the appraisal of stress, such as interoception.”
Aging is highly programmed all the way from conception to death, where the program finally kills every one of us one way or the other. Various interventions can tweak the program one way or the other. A very large number of these can kill us sooner. A precious few can keep us going healthily longer, and meditation appears to be one of those. So, if you are older and want to keep going healthily and happily, you might want to try it.


Pingback: The Amazing Power of NRF2 Boosters: Healing Your Mind Naturally - American Center for Natural Medicine
Pingback: The Amazing Power of NRF2 Boosters: Healing Your Mind Naturally - Dr Yas ND
Pingback: URL
Pingback: 21 benefits of meditation | Daily-Inspiration
Pingback: How Meditation Slows Aging: The Longevity Mindset, Part 4 - Garma On Health